NEW IDEAS ABOUT HYDRATION AND ITS IMPACT ON THE ATHLETE’S BRAIN, HEART AND MUSCLES
Published
July 2019
Author
José González-Alonso
Topics

KEY POINTS
- Dehydration is the process of losing body water through thermoregulatory sweating. It can lead to marked alterations in physiological function and decrements in athletic performance during training and competition in temperate and hot environments.
- Impaired endurance capacity in the severely dehydrated athlete is often associated with significant physiological strain in multiple systems, organs and tissues including the brain, heart and muscles.
- The physiological strain includes, but is not limited to, the ensuing high core temperature (hyperthermia); hyperventilation; decreased cardiac output; reduced blood flow to the active skeletal muscles, brain and skin; and alterations in cardiac function and contracting muscle and brain metabolism.
- Ingesting fluids during exercise and performing exercise at low intensities and/or in cold environments will attenuate or even prevent the aforementioned numerous effects of dehydration on physiological function and aerobic exercise performance.
- The physiological and performance impacts of dehydration are dependent on the environmental and exercise conditions. These should be considered in establishing the fluid replacement needs of the athlete.
INTRODUCTION
When people undertake prolonged exercise, they experience significant body fluid losses through thermoregulatory sweating and become progressively dehydrated. If dehydration is not attenuated via fluid replacement during exercise, physiological function and endurance capacity may be drastically impaired (Cheuvront & Kenefick, 2014; González-Alonso et al., 2008; Sawka et al., 2011). The extent to which global physiological function and athletic performance are impaired will depend upon the interplay among the level of dehydration, the intensity of exercise, the external environmental conditions and the athlete’s training and heat-acclimation status. Conceivably, the severely dehydrated, heat unacclimated and unfit endurance athlete, who is training or competing in a hot and humid environment, will experience the most deleterious physiological and performance effects. The mildly dehydrated, highly fit endurance athlete training and competing in a cold environment will be at the opposite end of the spectrum. Although this hypothesis has support in the literature (e.g., Corbett et al. 2018) and is discussed and substantiated below in respect to the influence of physiological demand, it is acknowledged that further research is warranted to establish how hydration level, physical fitness, heat acclimation and environmental conditions interact to differentially affect physiological function and endurance athletic performance.
Many insightful experimental approaches have been employed over the years to advance our understanding of the physiological factors limiting athletic performance in the dehydrated athlete (Sawka et al., 2011). One approach to be discussed in this Sports Science Exchange article has been to characterize the responses of the heart, active skeletal muscles and brain in order to establish whether “failure” in one or all of these organ systems underpins the development of fatigue in different hydration, environmental and exercise conditions (Trangmar & González-Alonso 2017, 2019). Accordingly, the aims of this article are: 1) to first characterize the impact of hydration and environmental conditions on submaximal and maximal endurance capacity in athletes, 2) to then describe the circulatory and metabolic consequences of dehydration and concomitant hyperthermia on the athlete’s heart, active muscles and brain, and 3) end with the practical implications of the further evolution of our understanding of the processes involved in the earlier onset of fatigue that occurs in the dehydrated athlete.
HYDRATION AND ATHLETIC PERFORMANCE
Endurance athletes such as marathon runners generally adopt strategies to compete at the highest pace they can sustain for the duration of the event. This ability to sustain a given pace or submaximal exercise intensity for prolonged periods (i.e., submaximal endurance capacity) can be drastically impaired in environmental conditions causing significant levels of dehydration and hyperthermia (Cheuvront & Kenefick, 2014; González-Alonso et al., 2008; Nybo et al., 2014; Sawka et al., 2011). The greatest impairments in submaximal endurance capacity occur in hot environments where athletes may experience profound degrees of dehydration and hyperthermia (Sawka et al., 2011). This is because body water losses due to sweating are high during prolonged moderate-to-intense exercise in hot environments (1.0–2.5 L/h) and the ensuing dehydration blunts heat dissipation (i.e., by impairing sweating and skin blood flow responses) and causes heat storage in the body with concurrent increases in core temperature (i.e., hyperthermia). Interestingly, athletes fatigue earlier in this scenario, despite the fact that whole-body aerobic metabolism ( O2) is preserved. This is a result of compensatory adjustments in oxygen extraction from the circulation (González-Alonso et al., 1998) (Figure 1), as discussed in the next section. The impact of dehydration on submaximal exercise performance is minimal when the environmental temperature is low (< 15°C) and skin and core temperatures are markedly reduced in comparison to hot, humid environments (Kenefick et al., 2010). As the effects of dehydration interact with those of hyperthermia, the magnitude of these physiological stressors and the overall functional demands of exercise need to be considered in predicting their impact on general physiological function and endurance capacity.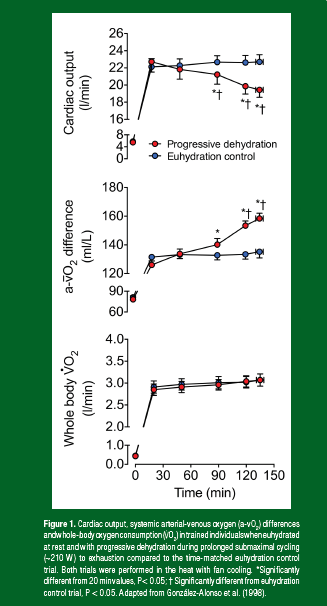
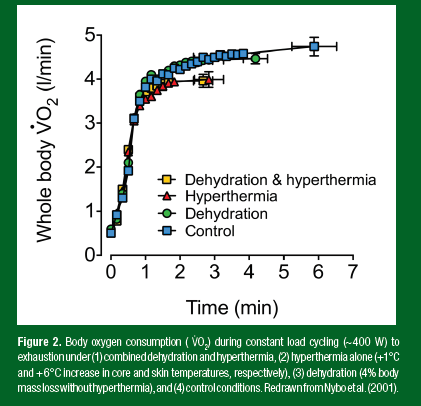
Endurance sporting events such as long road cycling stage races (or many team sports) include intermediate sprints where athletes rapidly increase their physiological demand to levels that may require near to maximal aerobic power ( O2max). This raises the question as to whether dehydration hinders physiological function and exercise performance at the maximal aerobic exercise domain (i.e., exhaustive exercise that can be sustained for 3–10 min; maximal endurance capacity). The magnitude of skin and core temperature elevations (i.e., whole-body hyperthermia) is again an important factor. As with submaximal exercise performance, low levels of dehydration (< 3% body mass loss) do not appreciably compromise O2max or maximal endurance capacity in cold environments, where the athlete experiences much lower skin and core temperatures (Cheuvront & Kenefick, 2014; Sawka et al., 2011). However, when dehydration occurs in temperate-to-hot ambient temperatures and whole-body hyperthermia becomes apparent, O2max and maximal endurance capacity are noticeably compromised (Ganio et al., 2006; Nybo et al., 2001).
Two studies using incremental and constant load exercise protocols illustrate the impact of whole-body dehydration and/or hyperthermia on O2max and maximal endurance capacity. During incremental exercise to exhaustion, O2max and work capacity were reduced by 9–12% when athletes were dehydrated by 4% of their body mass (i.e., ~3 kg in 75 kg athletes) following 120 min of submaximal exercise in the heat (Ganio et al., 2006). In contrast, when the loss in body mass was minimized (e.g., by shortening the duration of submaximal exercise), or when fluid was regularly ingested, no significant fall in O2max was observed. This phenomenon is also manifested during constant-load maximal exercise (i.e., 3–10 min) where muscle recruitment and metabolic demand are not changing as drastically as during incremental exercise. Nybo and collaborators (2001) had endurance-trained athletes perform 4 cycling bouts to exhaustion at ~400 W in a control and a hot environment, preceded by 2 h of submaximal cycling in the heat where hydration status was carefully manipulated to induce either 4% body mass loss (i.e., ~3 kg in 73 kg athletes), or a maintained hydration status by ingesting fluid during exercise. The combination of dehydration and hyperthermia and whole-body hyperthermia alone reduced O2max by 16% and endurance performance by ~52% compared to the control hydrated condition (Figure 2). Of note is the remarkably similar negative effects of whole-body hyperthermia evoked by circulating hot water through a suit in euhydrated subjects and combined dehydration and hyperthermia induced by prolonged exercise in the heat. The environments in which most sport competitions take place are different from the severe heat stress conditions induced in the laboratory with a water-perfused suit (uncompensable hot environments) (Chiesa et al. 2019). The impaired aerobic power and endurance capacity in compensable warm environments favoring evaporative cooling is more likely the result of the negative physiological effects of dehydration and hyperthermia. In support of this notion, when the athletes exercised in a dehydrated state, but in cool conditions affording the maintenance of low body temperatures, the fall in O2max and maximal endurance capacity were noticeably attenuated (6% and ~25%, respectively) (Nybo et al., 2001). In conclusion, dehydration levels amounting to 3–4% body mass loss, which athletes often experience during endurance events in compensable temperate-to-hot environments, promotes body hyperthermia and impairs submaximal and maximal endurance exercise capacity. These impairments are associated with an unchanged submaximal whole-body O2, but a markedly reduced O2max, indicative of an increased relative intensity during submaximal exercise reflected metabolically by enhanced reliance on muscle glycogen and cellular metabolism (González-Alonso et al., 1999a; Logan-Sprenger et al., 2013). In cold environments, however, similar levels of dehydration have smaller or minimal effects on aerobic metabolism and endurance exercise performance.
HYDRATION AND THE FUNCTION OF THE HEART, SKELETAL MUSCLES AND BRAIN
Endurance capacity is largely determined by the athlete’s ability to maintain a homeostatic state in which the respiratory, cardiovascular, metabolic, musculoskeletal, nervous and endocrine systems adequately meet the overall functional demands of exercise. This boils down to the capacity to maintain appropriate delivery of blood, oxygen and nutrients to and removal of metabolic by-products (including heat) from the heart, active muscles and brain, and all essential organs and tissues in the endurance athlete. The Fick principle sheds light on the integrative processes determining regional and systemic aerobic metabolism, which can be a determining factor limiting endurance capacity in some conditions. This principle states that the rate of oxygen uptake ( O2) by the human body, an organ, limb or tissue, is equal to the product of blood flow and the arterial-venous oxygen (a-vO2) content differences (Figure 3). It is important to recognize that a reduction in flow does not necessarily lead to reduced O2 if the a-vO2 difference proportionally increases. This relationship between blood flow and aerobic metabolism will therefore be examined below to evaluate whether reduced oxygen supply to, and aerobic metabolism by the human heart, active skeletal muscle and/or the brain could explain the accelerated fatigue and impaired aerobic exercise performance often seen in the dehydrated athlete.
Hydration and the Heart
A progressive fall in cardiac output is a key feature of the dehydration-induced cardiovascular strain observed during prolonged, strenuous whole-body exercise in temperate-to-hot environments (Hamilton et al., 1991; González-Alonso et al., 1995, 1998; Montain & Coyle 1992; Sawka et al., 1979). This response is prevented in trained and partially heat acclimated athletes by maintaining euhydration via ingestion of fluids during exercise (Hamilton et al., 1991; González-Alonso et al., 1995, 1998; Montain & Coyle 1992) (Figure 1). Concomitant with the declining cardiac output, heart rate rises continuously, whereas stroke volume declines by ~30% (González-Alonso et al., 1995, 1997), secondary to the rise in core body temperature and tachycardia and the loss in blood volume likely limiting the filling of the heart (Fritzsche et al., 1999; González-Alonso et al., 1997, 1999b,c, 2000). Importantly, reductions in systemic blood flow and oxygen delivery do not readily compromise submaximal whole-body O2 in the dehydrated endurance athlete because of the parallel compensatory adjustments in peripheral tissue and organ oxygen and substrate extraction from the circulation (Figure 1). Similar adjustments are expected to occur across the heart.

The early fatigue experienced by the dehydrated athlete during prolonged submaximal exercise is therefore unrelated to a blunted whole-body aerobic energy production but is closely coupled to high levels of core hyperthermia and alterations in muscle substrate and glycogen utilization and increases in muscle anaerobic metabolism and neural activation, possibly reflecting a mismatch between energy demand and production (González-Alonso et al. 1999a, 1999c).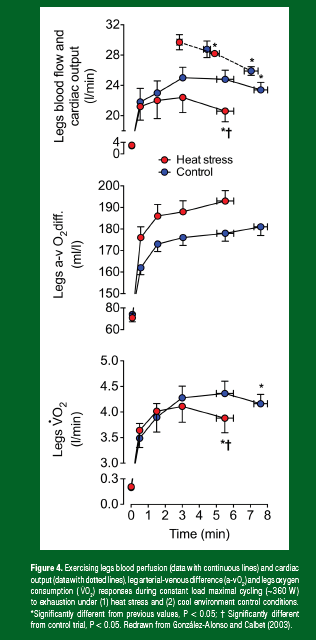
Whole-body hyperthermia alone, however, does not reduce stroke volume to the same extent, and a number of studies show that cardiac output is elevated during hyperthermic, submaximal exercise, rather than reduced (Pearson et al., 2011; Rowell et al., 1969; Stöhr et al., 2011a; Wilson et al., 2009). These contrasting findings suggest that compromised cardiac output is dependent on the extent of the cardiovascular challenge induced by combined stress evoked by dehydration, hyperthermia and exercise, which together set the overall functional demand. Studies assessing the impact of progressive dehydration on central and limb hemodynamics at rest and during exercise of a low physiological load (isolated-limb exercise) support this idea. Knee-extensor exercise following progressive dehydration reduced blood volume (~5%) and lowered stroke volume (~20 mL) to a similar degree to that seen in the whole-body exercise paradigm. The fall in stroke volume was coupled to a substantial fall in end-diastolic volume, with only a small fall in end-systolic volume and a marked elevation in heart rate (~30 beats/min) compared to control (hydrated) values. Intriguingly, however, and in contrast to whole-body exercise, cardiac output was maintained at rest and during exercise across all the hydration manipulations (Pearson et al., 2013; Stöhr et al., 2011b). Similarly, graded dehydration up to 4–5% of body mass loss does not compromise cardiac output during exercise in the cold, where skin and core temperature are significantly reduced (González-Alonso et al., 2000). Therefore, the physiological demands of the exercise (which can be substantially greater than those induced by dehydration alone or combined dehydration and low intensity exercise), play an important role in determining the severity of the cardiovascular strain and the metabolic and ultimately performance consequences of dehydration.
Hydration and Skeletal Muscles
When dehydrated, the skeletal muscle circulation mirrors the central hemodynamic alterations at rest and during exercise. At rest, limb blood flow is slightly, but significantly, enhanced with progressive dehydration, a response maintained during submaximal small muscle mass exercise (i.e., single leg knee-extensor exercise), despite substantial body mass losses (~3.5%) (Pearson et al., 2013). These are conditions in which the overall physiological strain imposed by dehydration is relatively small because the majority of the body’s physiological systems are working substantially below their functional capacities. Conversely, during prolonged, submaximal whole-body exercise (i.e., two leg cycling), the substantial fall in cardiac output (~4 L/min) is associated with a ~2 L/min reduction in contracting limb blood flow compared to control euhydrated exercise in the heat (González-Alonso et al., 1998). The marked fall in active limb blood perfusion during whole-body exercise is offset when fluid intake matches fluid loss (González-Alonso et al., 1998; Nielsen et al., 1990), and when systemic hemodynamics are normalized (compared to upright control conditions) by exercising in a supine or semi-recumbent position, despite significant whole-body hyperthermia (González-Alonso et al. 1999b; Nielsen et al., 1993). During submaximal upright exercise, reductions in contracting limb and systemic blood flow with dehydration and hyperthermia are associated with proportional increases in oxygen extraction such that O2 is maintained (Figure 1). This is not the case, however, during maximal aerobic exercise where the muscle oxygen extraction reserve of skeletal muscle is too small to fully compensate for large reductions in oxygen supply and, as a result, locomotor muscle and systemic O2 declines with dehydration and hyperthermia, whole-body hyperthermia and even during control conditions (Figures 2, 4). The magnitude of body mass loss (dehydration) in the aforementioned studies inducing marked physiological strain and performance decrements approached or reached 4%. It should be recognized that attenuating dehydration via fluid ingestion during exercise reduces physiological strain (Montain & Coyle, 1992; González-Alonso et al., 2000; Figure 5) while more severe dehydration could exacerbate such a phenomenon. Taken together, the contracting limb and systemic hemodynamic responses to dehydration are intimately linked, such that limb vasoconstriction may lead to compromised cardiac output through reductions in venous return, left ventricular filling and ultimately stroke volume. It is also clear that the large fall in active skeletal muscle blood perfusion during strenuous whole-body exercise can reduce oxygen supply to the muscle, which is initially compensated by increases in oxygen extraction early in maximal exercise and during prolonged submaximal exercise, but will lead to compromised local and systemic aerobic metabolism and accelerated fatigue during maximal exercise (Ganio et al., 2006; González-Alonso & Calbet, 2003; Nybo et al., 2001). A compensatory increase in anaerobic ATP production can be sustained only for a short period due to the low capacity of the anaerobic energy pathways. This suggests that a mismatch between energy demand and supply is a likely factor leading to fatigue during maximal endurance exercise in the athlete regardless of the hydration status.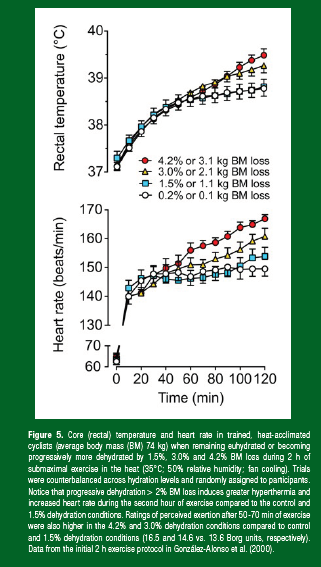
Hydration and the Brain
Dynamic exercise requires the activation of motor and cardiorespiratory neural centers in the brain. Because increases in cerebral blood flow and oxygen and nutrient supply might be needed to meet the presumed greater “brain metabolic activity” (Nybo et al., 2002; Trangmar et al., 2015), any factors compromising cerebral blood flow may compromise motor neuron activation and exercise capacity. At rest, elevations in core temperature of 1.5°C reduce cerebral blood flow by ~15% (Ogoh et al., 2013), whereas dehydration without concomitant hyperthermia elevates brain blood perfusion (Fan et al., 2008). Combined hyperthermia and dehydration also alter cerebral blood flow during different types of exercise. For example, cerebral blood flow is suppressed throughout the duration of self-paced (time trial) exercise/ effort, or markedly reduced by ~15–25% when hyperthermia develops in an uncompensable condition, compared to the same task in a cool or thermoneutral environment (Nybo & Nielsen, 2001; Nybo et al., 2002; Périard & Racinais, 2015). The development of dehydration (> 3% body mass loss) during prolonged exercise in the heat causes further cerebrovascular instability by hastening the decline in cerebral blood flow, concomitantly to elevated hyperthermia, hyperventilation, hypocapnia (a reduction in the potent cerebral vasodilator CO2), tachycardia and early fatigue (Trangmar et al., 2015). In contrast, the reduction in cerebral blood flow is attenuated when fluid intake matches body fluid loss through sweating (Trangmar et al., 2015).
The effect of hyperthermia and dehydration on cerebral blood flow is not isolated to prolonged exercise, as the typically observed fall in cerebral blood flow during severe-intensity exercise is accelerated (i.e., occurring at lower work rate or shorter duration of exercise) in uncompensable environmental conditions (González-Alonso et al., 2004; Trangmar et al., 2017). This is also the case when dehydrated athletes perform incremental exercise in a compensable hot environment (Trangmar et al., 2014), where dehydration and concomitant hyperthermia reduce cerebral blood flow to values equivalent to control conditions, but at a significantly lower absolute exercise intensity. The cerebral blood flow dynamics are, however, normalized to control conditions when participants maintain their normal hydration status (González-Alonso et al., 2004).
In summary, exercising in the heat, evoking severe body hyperthermia, compromises cerebral perfusion during strenuous submaximal and maximal endurance exercise. The development of dehydration exacerbates the cerebrovascular strain and accentuates the fall in cerebral blood flow. Despite the marked fall in cerebral blood flow, however, the global O2 of the brain is not compromised at any level of exercise intensity due to compensatory elevations in brain oxygen extraction (Trangmar et al., 2014, 2015). Thus, reduced brain oxygen consumption is unlikely to contribute to the fall in maximal aerobic power and endurance performance in the dehydrated athlete.
PRACTICAL APPLICATIONS
- Ingestion of fluids during prolonged exercise reduces the physiological strain and the decrements in athletic performance that occur with progressive dehydration during training and competition in temperate and hot environments.
- Most sport competitions take place in environmental conditions favoring evaporative cooling where increases in skin and core temperatures and decrements in athletic performance are not as large as seen with severe heat stress in laboratory conditions where convective air flow is minimal.
- The impaired submaximal and maximal endurance capacity in compensable environments favoring evaporative cooling is likely the result of the numerous physiological effects of dehydration and concomitant hyperthermia.
- Performing exercise at low intensities and/or in cold environments not only reduces the fluid replacement needs, but also diminishes the physiological and physical performance consequences of any given level of dehydration.
- The fluid replacement needs of the athlete vary significantly because the physiological strain placed upon the heart, active muscles and brain differs depending on the environmental and exercise conditions.
- During training and competition in the heat, however, the endurance athlete is likely to experience greater physiological strain with increasing levels of dehydration compared to being mildly dehydrated or maintaining euhydration.
SUMMARY
Severe dehydration and hyperthermia impair submaximal and maximal endurance performance. The impaired aerobic exercise performance is associated with a myriad of alterations in physiological function including reduced oxygen delivery to multiple body tissues and organs, enhanced reliance on muscle glycogen and cellular metabolism, changes in neural activity and, in some exercise and environmental conditions requiring near to maximal functional capacity, compromised muscle and whole-body aerobic capacity. It is evident, however, that the level of dehydration, the intensity of the exercise and the external environmental conditions determine the extent to which general physiological function is compromised. Dehydration and hyperthermia can elevate blood flow to the heart, active muscles and brain at rest and during low-intensity exercise. When exercise intensity is increased above moderate levels or when exercise duration is prolonged, contracting limb muscle, brain and systemic blood flow gradually declines (Figures 1, 2, 4). This diminished peripheral blood flow has a different effect on regional tissue aerobic metabolism, where compromised active muscle blood flow results in a decreased O2, but brain and heart aerobic metabolism is preserved. This decreased contracting skeletal muscle O2 is a likely precursor to early fatigue when severe intensity exercise is performed in hot environments and the athlete experiences marked dehydration and hyperthermia (Figure 3).
ACKNOWLEDGEMENTS
The author would like to thank all the participants and research students and collaborators for their contributions to some of the studies reviewed here.
REFERENCES
Cheuvront, S.N., and R.W. Kenefick (2014). Dehydration: physiology, assessment, and performance effects. Compr. Physiol. 4:257-285.
Chiesa, S.T., S.J. Trangmar, K. Watanabe, and J. González-Alonso (2019). Integrative human cardiovascular responses to hyperthermia. In: J.D. Périard and S. Racinais (eds.) Heat Stress in Sport and Exercise. Springer, Cham. p. 45-65.
Corbett, J., R.A. Rendell, H.C. Massey, J.T. Costello, and M.J. Tipton (2018). Inter-individual variation in the adaptive response to heat acclimation. J. Therm. Biol. 74:29-36.
Fan, J.L., J.D. Cotter, R.A. Lucas, K. Thomas, L. Wilson, and P.N. Ainslie (2008). Human cardiorespiratory and cerebrovascular function during severe passive hyperthermia: effects of mild hypohydration. J. Appl. Physiol. 105:433-445.
Fritzsche, R.G., T.W. Switzer, B.J. Hodgkinson, and E.F. Coyle (1999). Stroke volume decline during prolonged exercise is influenced by the increase in heart rate. J. Appl. Physiol. 86:799-805.
Ganio, M.S., J.E. Wingo, C.E. Carroll, M.K. Thomas, and K.J. Cureton (2006). Fluid ingestion attenuates the decline in O2 peak associated with cardiovascular drift. Med. Sci. Sports Exerc. 38:901-909.
González-Alonso, J., and J.A. Calbet (2003). Reductions in systemic and skeletal muscle blood flow and oxygen delivery limit maximal aerobic capacity in humans. Circulation. 107:824-830.
González-Alonso, J., R. Mora-Rodríguez, P.R. Below, and E.F. Coyle (1995). Dehydration reduces cardiac output and increases systemic and cutaneous vascular resistance during exercise. J. Appl. Physiol. 79:1487-1496.
González-Alonso, J., R. Mora-Rodríguez, P.R. Below, and E.F. Coyle (1997). Dehydration markedly impairs cardiovascular function in hyperthermic endurance athletes during exercise. J. Appl. Physiol. 82:1229-1236.
González-Alonso, J., J.A. Calbet, and B. Nielsen (1998). Muscle blood flow is reduced with dehydration during prolonged exercise in humans. J. Physiol. 513:895-905.
González-Alonso, J., J.A.L. Calbet, and B. Nielsen (1999a). Metabolic and thermodynamic responses to dehydration-induced reductions in muscle blood flow in exercising humans. J. Physiol. 520:577-589.
González-Alonso, J., R. Mora-Rodríguez, and E.F. Coyle (1999b). Supine exercise restores arterial blood pressure and skin blood flow despite dehydration and hyperthermia. Am. J. Physiol. 277:H576-H583.
González-Alonso, J., C. Teller, S.L. Andersen, F.B. Jensen, T. Hyldig, and B. Nielsen (1999c). Influence of body temperature on the development of fatigue during prolonged exercise in the heat. J. Appl. Physiol. 86:1032-1039.
González-Alonso, J., R. Mora-Rodríguez, and E.F. Coyle (2000). Stroke volume during exercise: interaction of environment and hydration. Am. J. Physiol. 278:H321-H330.
González-Alonso, J., M.K. Dalsgaard, T. Osada, S. Volianitis, E.A. Dawson, C.C. Yoshiga, and N.H. Secher (2004). Brain and central haemodynamics and oxygenation during maximal exercise in humans. J. Physiol. 557:331-342.
González-Alonso, J., C.G. Crandall, and J.M. Johnson (2008). The cardiovascular challenge of exercising in the heat. J. Physiol. 586:45-53.
Hamilton, M.T., J. González-Alonso, S.J. Montain, and E.F. Coyle (1991). Fluid replacement and glucose infusion during exercise prevent cardiovascular drift. J. Appl. Physiol. 71:871-877.
Kenefick, R.W., S.N. Cheuvront, L.J. Palombo, B.R. Ely, and M.N. Sawka (2010). Skin temperature modifies the impact of hypohydration on aerobic performance. J. Appl. Physiol. 109:79-86.








