Acute Weight Management in Combat Sports: Pre Weigh-In Weight Loss, Post Weigh-In Recovery and Competition Nutrition Strategies

KEY POINTS
- Combat (and other weight category) sports athletes commonly reduce body mass in an effort to compete in weight divisions below their day-to-day training weight.
- Both chronic and acute weight losses (often in the form of extreme dehydration) are commonly used to “make weight.” These practices correlate with competitive success in certain sports; however, they can be detrimental to one’s health and absolute physical performance if not sensibly implemented.
- By strategically manipulating dietary intake of fiber, carbohydrate, sodium and fluid, athletes can minimize the requirement for sweating to make weight and the associated health risks of excessive dehydration.
- Athletes should develop a thorough understanding of the optimal nutritional strategies involved in recovery and combine them with practices identified as making them “feel good.” Preferably, they should focus on suitable carbohydrate sources and appropriate fluid intakes in the form of familiar foods trialed ahead of competition.
- Athletes should plan their weight-making strategy ahead of time and practice this prior to important competitions. Furthermore, athletes should evaluate and refine their weight-making and recovery practices from competition to competition.
INTRODUCTION
In most combat sports, competitors are separated into weight divisions in an attempt to “create an even playing field.” Prior to competition, athletes must attend an official “weigh-in” and have their body mass (BM) verified to ensure they have “made weight.” The period of time between weigh-in and competition differs between combat sports, however a recovery period of at least 3 and up to 24 h exists among the Olympic combat sports and an even greater time (>30 h) may be available in professional combat sports. Most fighters try to take advantage of this scenario by using acute weight loss (AWL) strategies (cutting weight) in the hours and days before weigh-in, temporarily lowering their BM to make weight at a lower division than their day-to-day weight (and thus compete against smaller opponents). Athletes then attempt to reverse the negative performance effects of AWL during the recovery period (Franchini et al., 2012). Indeed, there is indirect evidence indicating AWL increases success in some combat sports (Franchini et al., 2012; Reale et al., 2017a). Thus if sensibly implemented, and adequate post weigh-in recovery opportunities exist, cutting weight might be seen as a pragmatic way to optimize competitiveness.
It needs to be stated that severe health consequences (including death [Centers for Disease Control and Prevention, 1998]) may arise from extreme and excessive AWL. Thus, the magnitude and methods of AWL need to be managed in such a way as to minimize potential negative consequences. Although some have called for the abolishment of weight cutting, until such time that regulations specifically and systematically prohibit the practice, it appears athletes will continue to cut weight. Therefore, sports nutrition professionals need to pragmatically balance athletes’ desires to achieve (real or perceived) advantages with concerns for their physical, mental and emotional safety. This means advising against excessively large magnitudes of weight loss and educating both athletes and coaches to make use of less harmful, evidenced based methods of weight loss, as well as optimizing recovery.
Achievable magnitudes of safe acute weight loss
Combat sport athletes commonly lose ≥ 5% BM in the week prior to weigh-in (Franchini et al., 2012). Under some conditions, achieving 5% and up to 8% BM losses alongside acceptably small impacts on health and performance may be possible (Reale et al., 2016, 2017a). However, an appreciation of optimized methods of AWL, as well as a realistic assessment of one’s “starting point” prior to AWL is required. Utilizing solely dehydration to achieve 5 - 8% BM loss is unadvisable and dangerous to health. Instead, a calculated manipulation of gut content, carbohydrate stores and finally body water should be utilized in order to achieve the desired AWL. Therefore, the starting point prior to AWL should represent a BM associated with a euhydrated, well-nourished state, which allows an opportunity for sizeable manipulation of these compartments. Lastly, the recovery time available post weigh-in/pre-competition will further determine the magnitude of AWL achievable if one wants to present to competition in an acceptable state. As a guide, with greater than 12 h between weigh-in and competition (e.g., sports which conduct weigh-ins the day before competition), a fully hydrated, well-nourished athlete may lose and recover from up to 8% BM (Reale et al., 2016). Those weighing-in the morning of competition (with limited recovery time, e.g. ≤ ῀6 h) should aim for no more than 5% BM acute losses (Reale et al., 2016).
Methods to Achieve Safe Acute Weight Loss
Manipulation of Gut Content
Combat sport athletes commonly fast, limit portion sizes or reduce total food volume prior to weigh-in to reduce the mass of intestinal contents and thus total BM (Brito et al., 2012; Fleming & Costarelli, 2007; Franchini et al., 2012). Laxative and bowel preparation formula use is common among weight category sport athletes (Brito et al., 2012; Franchini et al., 2012). While this method is effective in removing intestinal bulk and cleansing the bowel, this will also impact on energy and macronutrient intake/absorption, and has been shown to reduce exercise capacity (Holte et al., 2004). Therefore, dietary strategies which reduce total food volume without impacting energy and macronutrient intake (i.e., the consumption of low weight, energy dense foods in the hours and days prior to weigh-in) are preferable. This is especially true for athletes who have limited time to effectively rehydrate and refuel prior to competition (due to limited recovery time post weigh-in).
Certain types of dietary fiber can both slow gut transit times of foods as well as draw water into the intestinal space, “bulking” stools. Different foods possess different fecal bulking properties (Monro, 2000), thus if one reduces the consumption of “bulking” fiber-rich foods, a reduction of undigested plant matter within the gut and a reduction in water drawn into the intestinal space follows. This decreases fecal bulk, total gut contents and overall BM. In fact, a linear relationship exists between fiber intake and bowel cleanliness. The consumption of a low fiber diet for just two days begins cleansing the bowel (Wu et al., 2011), with seven days being as effective as a bowel preparation formula, while resulting in less physiological stress than bowel preparation formulas (Lijoi et al., 2009).
Limited research examining low fiber diets in the context of AWL exists, and whole gut transit times vary widely between individuals from 10 - 96 h (Lee et al., 2014). Therefore, precise guidelines for the use of fiber restriction for AWL cannot presently be determined. However, indirect evidence suggests significant weight loss (῀1.5% BM), in line with that following bowel preparation formula use (Holte et al., 2004), is achieved following 48 h of fiber restriction (≤ 10 g/d), with no further significant losses in most individuals (Reale et al., 2017b). Thus, 48 h seems a sensible starting point to implement this approach, noting that individual responses may vary and some individuals may benefit from a restriction > 48 h.
Manipulation of Glycogen Content
Dietary carbohydrate is stored in skeletal muscle and the liver as glycogen and these energy reserves can be mobilized to meet the demand for glucose. Glycogen is noted to bind to water at a ratio of 1:2.7 (Bergström & Hultman, 1972). Given the substantial glycogen storage capacity of athletes, and the ability to manipulate these stores (Burke & Deakin, 2009), this represents another AWL strategy available to the weight category sport athlete. Both the restriction of dietary carbohydrate coupled with glycogen demanding training, and the increase of training alongside one’s habitual carbohydrate intake, will result in changes in glycogen status. Prior to weigh-in/competition, athletes tend to decrease (not increase) training, and therefore reducing (or restricting altogether) carbohydrate intake without increasing training in order to deplete glycogen stores would be a logical strategy. It has been shown that 7 d of a low carbohydrate diet (< 50 g/d), combined with training and a minor energy deficit (< 10%) can achieve a ~2% BM reduction while maintaining strength, power and anaerobic capacity measures (Sawyer et al., 2013). However, the exact magnitude of possible BM loss, the degree of carbohydrate restriction and the time frame required, will depend on one’s glycogen status and training load prior to dietary restriction. A general recommendation of < 50 g/d for 3-7 d for combat sport athletes wanting to deplete glycogen prior to weigh-in has been suggested (Reale et al., 2016). Athletes should consider the time available post weigh-in to refuel and the requirements of their sport (i.e., fuel demands, need for repeated weigh-ins, etc.) when deciding whether to utilize glycogen depletion (and to what extent) as a means to achieve AWL.
Manipulation of Body Water
Water constitutes ~60% of the human body (Sawka et al., 2005) in the general population and likely more in athletes due to higher amounts of lean mass. Given the size of this body compartment and the short time frame in which fluctuations can occur, it is no surprise that dehydration is the primary AWL strategy used by many combat sport athletes. Although mild dehydration (< 2% BM) is unlikely to affect relevant performance, larger magnitudes may be problematic, particularly when limited time to rehydrate post weigh-in exists (Reale, 2016, 2017a). Put simply, athletes have two methods available to them to decrease body water; consume less fluid and/or excrete more fluid. A 24 h fluid restriction (< 300 ml (10 oz)) may result in 1.5 - 2% BM loss (James & Shirreffs, 2013); however, athletes commonly achieve losses greater than this following increased sweating via both active (exercise induced) and/or passive methods (i.e., saunas, heated environments, etc.) (Franchini et al., 2012).
It is important to note the differing physiological responses of passive and active sweating. Passive sweating prior to exercise decreases plasma volume, sweat rate and stroke volume, contributing to increased serum osmolality, heart rate and body heat storage, whereas this happens to a lesser extent following active sweating (Walsh et al., 1994). Therefore, a combination of fluid restriction and active sweating (preferably accompanying existing training sessions in the hours or day prior to weigh-in) may be the most pragmatic, performance preserving method to achieve AWL via dehydration. Additional passive sweating should only be used when necessary and when sufficient recovery time is available. If using a sauna to facilitate perspiration, dry heat should be used in preference to steam saunas, as this results in greater fluid losses for a given period of time and less physiological strain (Pilch et al., 2014).
Lastly, reductions in sodium intake may also result in body water losses, resulting from renal attempts to maintain osmotic pressure, achieved through the excretion and retention of both electrolytes and fluid. BM losses of 1-2% have been reported in hypertensive subjects who switched to a low sodium (< 500 mg) diet for 5 days (He et al., 2001); however, no interim BM measures were taken, so it is not possible to state the exact time frame of weight loss. Furthermore, whether or not similar losses would occur in normotensive subjects is unknown. Despite the lack of definitive evidence, reductions in sodium intake during AWL are common (Fleming & Costarelli, 2007), and perhaps even if a reduction in sodium intake may not influence total body water per se, when used in combination with other fluid manipulation strategies it may “release” more body water and allow a reduction in BM (Reale et al., 2016).
Post weigh-in recovery nutrition
Any advantage gained from cutting weight leading into competition will be best maximized by enacting a calculated recovery plan following weigh-in. Priorities following weigh-in may include rehydration, glycogen restoration and the management of gastrointestinal distress.
Rehydration
Combat sport athletes should aim to restore fluid losses to within ~2% of “pre-hypohydration” BM in order to minimize negative performance effects (Burke & Deakin, 2009; Walsh et al., 1994). Factors which may prohibit the attainment of this goal include insufficient recovery time and difficulty in accurately identifying the magnitude of hypohydration, since acute changes in BM (traditionally thought to mirror fluid losses) will likely be made up of more than solely body water. Adequate recovery time following weigh-ins conducted the day before competition is likely, however this may not be the case for those weighing-in the morning of competition. Therefore, those who weigh-in the morning of competition may best manage BM by preventing the need to lose > 3% BM via dehydration in order to make weight (Reale et al., 2016, 2017a).
General sports nutrition recommendations suggest 125 - 150% of any fluid deficit needs to be ingested to compensate for continued urine losses (Shirreffs & Maughan, 1998; Maughan & Leiper, 1999; Burke & Deakin, 2009). In certain situations this may be difficult to implement since the true fluid deficit may be unknown (e.g., “non-fluid” AWL may confound the typical use of BM changes in estimating hypohydration) and large fluid volumes may be impractical to consume during limited recovery time. In addition to fluid volumes larger than losses, athletes can further enhance rehydration efforts post weigh-in via additional strategies.
Consuming a large fluid bolus ~600 – 900 mL (20 – 30 oz) immediately post weigh-in as well as additional boluses at regular intervals will maintain a high gastric volume, in turn speeding gastric emptying and potentially preventing the need to consume fluids closer to competition (Maughan & Leiper, 1999).
Sweat losses are comprised of not only fluid but electrolytes, (primarily sodium and chloride) (Maughan & Leiper, 1999). Thus, replacement of these electrolytes will promote restoration of plasma osmolality and volume. Sweat sodium concentrations range from ~20 - 80 mmol/l (Shirreffs & Maughan, 1998; Maughan & Leiper, 1999, Burke & Deakin, 2009), making it difficult to prescribe one “optimal” sodium concentration for a rehydration beverage. However, fluid retention does correlate with sodium content due to both electrolyte replacement and the effects on intestinal absorption (Maughan & Leiper, 1999). This occurs following both the consumption of salty foods alongside fluids (Ray et al., 1998) and sodium containing fluids alone. Sports drinks typically contain < 30 mmol/l sodium, whereas oral rehydration solutions (ORS), commonly used in the treatment of acute diarrhea or vomiting contain 50-90 mmol/l sodium (Maughan & Leiper, 1999; Burke, 2009). Thus, consuming beverages with additional sodium may be the best option when rehydration is the priority. Alternatively, consuming salty snacks alongside sports drinks will increase the total sodium load ingested, thereby increasing fluid retention. In this scenario, consideration needs to be given to the fact that increased energy derived from any food consumed concurrent to a sports drink will slow gastric emptying (Maughan et al., 1996). Lastly, fluid restriction (as opposed to dehydration following sweating) causes a decrease in net body water without the same electrolyte losses (James & Shirreffs, 2013). Therefore, electrolyte replacement is less important in this situation and lower sodium fluids will be well retained.
Glycogen Restoration
Fully saturated glycogen stores may not be required for optimal performance in combat sports, however incomplete glycogen depletion impaired anaerobic exercise lasting ~5 min, and performance improvements following glycogen-loading in predominantly anaerobically fueled scenarios have also been noted (Pizza et al., 1995). Furthermore, BM gain (a consequence of glycogen loading) (Sawyer et al., 2013) may indirectly increase competitive success (Franchini et al., 2012; Reale et al., 2017a). Therefore, post weigh-in recovery nutrition should include enough carbohydrate to at least provide adequate fuel for competition needs, and potentially maximize glycogen stores (if time permits and intake does not interfere with rehydration or gastrointestinal (GI) comfort).
General sports nutrition guidelines prescribe carbohydrate intakes of 5-7 g.kg-1.d-1 for athletes engaged in moderate volume training and up to 7-10 g.kg-1.d-1 to maximize glycogen storage (Burke & Deakin, 2009; Burke et al., 2017). Taking into consideration tapered training and allowing for potential carbohydrate loading, a post weigh-in recommendation of 5-10 g/kg BM encompasses both goals. Those with limited recovery time and/or those wanting to avoid potential GI discomfort may want to aim for the lower end of this range, whereas athletes with extended recovery times and/or the desire to increase BM would likely benefit from consuming at the higher end. Selecting high glycemic index carbohydrate and/or carbohydrate-rich fluids (which simultaneously aide in rehydration efforts) may reduce GI discomfort commonly associated with the consumption of solid foods close to competition (Burke & Deakin, 2009; Reale et al., 2017a). Adding protein to recovery meals/snacks may increase glycogen storage when carbohydrate intake is sub-optimal (Ivy et al., 2002; Burke et al., 2017). Consideration needs to be given to rehydration however, as hypertonic fluids (e.g., fluids > 10% carbohydrate) may decrease the rate of gastric emptying and rehydration, as well as affect GI comfort (Evans et al., 2009). Therefore, at times, athletes may need to determine which takes priority between rehydration and refueling, as focusing on one may limit their ability to achieve the other.
Managing Gastrointestinal Distress
Ideally, post weigh-in intake should fully recover nutritional status while avoiding GI distress. Of the aforementioned AWL strategies, a low fiber diet is likely the least harmful (Reale et al., 2016). In contrast to depleted glycogen and dehydration, reduced GI bulk is not thought to be performance limiting, providing energy intake is adequate (Reale et al., 2016). Thus, BM loss by reducing gut contents does not require acute replacement, and recovery should focus on replacement of fluid and carbohydrate as dictated by acute losses. In fact, a sudden reintroduction of dietary fiber slows gastric emptying and nutrient absorption (Hillemeier, 1995), potentially producing GI discomfort (Mahan & Escott-Stump, 2008). The same occurs with large fat intakes (Mahan & Escott-Stump, 2008). Thus, dietary fiber and fat should be limited as consumption post weigh-in not only displaces other more important nutrients but may impair competition performance directly and indirectly. This consideration is heightened when the recovery period is limited.
Some athletes that are worried about GI distress (potentially worsened by gut contact during competition), may feel unable to consume solid foods or even energy containing fluids pre-event. For these (and all) athletes, there are options which may enhance performance without aggravating GI symptoms. Both caffeine use, and “mouth rinsing” and spitting of a carbohydrate based solution or food is known to aide performance during times of low carbohydrate availability (Kasper et al., 2016).
Becoming familiar with individual responses to caffeine is important; however, in general, the dose response relationship with caffeine follows a U-shaped curve. That is; mild to moderate doses (3–6 mg/kg) consumed 60 min pre-exercise elicits desirable effects, and increasing doses cause over stimulation, anxiety and potential decrements in fine motor control (Burke & Deakin, 2009).
Although no specific combat sports data exists, based on the current literature in comparable as well as wider scenarios, rinsing the mouth for ~10 s with a sports drink (or other carbohydrate solution or food) pre-competition may enhance performance (Burke & Maughan, 2015; Kasper et al., 2016). This represents a low risk strategy potentially providing increased drive, due to the activation of regions or responses in the central nervous system which may increase corticomotor activity and/or reduce perception of effort, at a time when athletes may want to avoid swallowing foods or fluids (Burke & Maughan, 2015).
Pre-competition nutrition
In most sports, pre-competition nutrition involves a “fine tuning” of nutritional status alongside the pursuit of comfort, routine and ritual practices and not the aggressive reversal of weight-making efforts. This represents another challenge for the combat sport athlete. Ideally, full recovery of nutritional status (following AWL) will occur several hours before competition, allowing one to focus on “traditional” pre-competition practices. When there is limited recovery time post weigh-in or when excessive AWL has occurred, incorporating these two themes can be challenging. Consequently, the shorter the time interval between weigh-in and competition, the less weight an athlete should attempt to lose/gain acutely.
Increased carbohydrate availability in the hours prior to exercise is a well-recognized strategy to improve performance across multiple sports (Lambert et al., 1991, Burke & Deakin, 2009). Determining specific pre-fight meal prescriptions is challenging at this stage; however, carbohydrate intakes ≥ 1g/kg in the hours before exercise are noted to assist repeated high intensity efforts (Lambert et al., 1991). Although athletes’ individual preferences must be considered, easily digested, low-fat, low-fiber carbohydrate-rich foods before and between bouts would seem ideal (Reale et al., 2017a, Burke & Deakin, 2009).
Managing post weigh-in recovery, gut comfort and competition nutrition concurrently
Post weigh-in there is a “crossover” time point where nutrition priorities change from recovery to competition (nutritional, mental and physical) preparation. For athletes who weigh-in the day prior to competition, achieving recovery goals prior to sleep makes sense, thus permitting a focus on competition preparation upon waking. For athletes weighing in on the morning of competition, isolating this crossover point is harder and is likely dictated predominantly by a desire to avoid gut discomfort and other anxieties surrounding the pre-competition period.
Assessment of recovery requirements and preparation of/access to appropriate fluids and foods should take place ahead of time, allowing recovery to begin immediately post weigh-in. There may be a conflict between rehydration goals where lower osmolality/energy beverages enhance gastric emptying and nutrient restoration goals where aggressive carbohydrate replenishment may slow gastric emptying. In this situation, athletes may need to make specific decisions regarding nutrition priorities. Fighters commonly select fluids in the period immediately (30-60 min) post-weigh-in, thus ingestion of an ORS (or a high sodium containing sports drink) may be a suitable choice for those prioritizing rehydration, whereas traditional sports drinks, gels, chews and candy or other high glycemic index foods that are portable and easily digested carbohydrate sources provide a post weigh-in solution targeted toward fueling. Further, liquid boluses aimed to maximize gastric volume/emptying could include sweetened milk to provide protein and carbohydrate simultaneously and thus address additional nutrition goals, but again decisions may need to be made regarding the importance of recovering fluid vs. carbohydrate/energy.
In the second hour of recovery, athletes may wish to begin solid food consumption. Carbohydrate-rich, low fiber, low fat selections will best promote glycogen storage while lessening potential GI discomfort. Continuing fluid intake during this time is also important, but if water is consumed alongside sodium-rich foods, electrolyte-containing beverages may not be required (Maughan et al., 1996). In reality, many common foods are either high in sodium and/or easy to add salt to, and are suitable as recovery meals (Ray et al., 1998). When controlling food composition is difficult and/or an athlete does not want to/or cannot eat a larger meal, continuing to drink an ORS to address hydration alongside sugar-rich snacks or sports foods will address carbohydrate requirements. Similarly, many sports drinks are convenient choices for moderate rates of rehydration and refueling. However, some have lower than optimal sodium contents for facilitating rapid rehydration, so consuming salty snacks concurrently will further support fluid retention. Proactive strategies addressing rehydration and glycogen replenishment should continue until recovery is achieved (e.g., consumption of 125-150% of fluid deficit and adequate carbohydrate) or until continued consumption causes GI distress or interferes with competition preparation.
Practical applications and summary
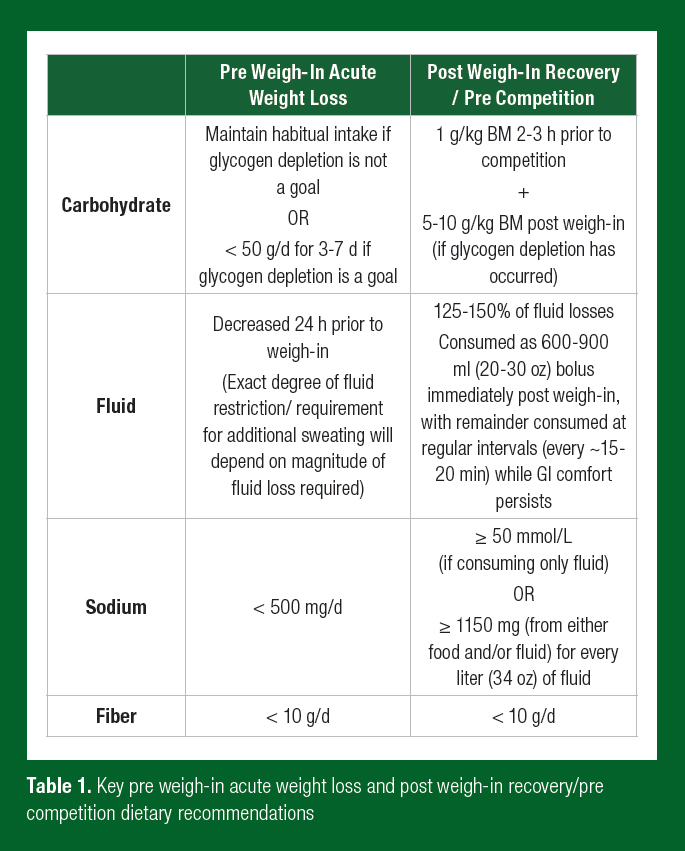
Weight cutting in combat sports is a contentious issue. It may indirectly increase competitive success while concurrently decrease absolute performance and present a health risk. Athletes should familiarize themselves with the associated risks and the evidenced based methods to manage them. Avoiding extreme magnitudes of acute weight (and in particular body water) fluctuations will best preserve performance and health. The table below summarizes key pre and post weigh-in nutrition recommendations, but it must be noted that exact requirements will vary based on magnitude of weight loss required, recovery time frame available post weigh-in, and requirements of the sport (Table 1). Combat sport athletes are advised to develop a plan that includes well-practiced routines, as well as continually evaluating and refining AWL and recovery processes throughout their career. For further detailed recommendations, readers are directed to existing acute weight loss (Reale et al., 2016) and recovery/pre-competition (Reale et al., 2017a) reviews.
References
Bergström, J., and E. Hultman (1972). Nutrition for maximal sports performance. J. Am. Med. Assoc. 221:999-1006.
Brito, C.J., A.F.C.M. Rosa, I.S.S. Brito, J.C.B. Marins, C. Cordova, and E. Franchini (2012). Methods of body-mass reduction by combat sport athletes. Int. J. Sport Nutr. Exerc. Metab. 22:89-97.
Burke, L.M. and V. Deakin (2009). Clinical Sports Nutrition. Sydney, Australia, McGraw-Hill Book Company.
Burke, L.M., and R.J. Maughan (2015). The Governor has a sweet tooth–mouth sensing of nutrients to enhance sports performance. Eur. J. Sports. Sci. 15:29-40.
Burke, L.M., L.J. van Loon, and J.A. Hawley (2017). Postexercise muscle glycogen resynthesis in humans. J. Appl. Physiol. 122:1055-1067.
Centers for Disease Control and Prevention (1998). Hyperthermia and dehydration-related deaths associated with intentional rapid weight loss in three collegiate wrestlers—North Carolina, Wisconsin, and Michigan, November–December 1997. MMWR Morb Mortal Wkly Rep. 47(6):105–108.
Evans, G.H., S.M. Shirreffs, and R.J. Maughan (2009). Acute effects of ingesting glucose solutions on blood and plasma volume. Br. J. Nutr. 101:1503-1508.
Fleming, S., and V. Costarelli (2007). Nutrient intake and body composition in relation to making weight in young male Taekwondo players. Nutr. Food Sci. 37:358-366.
Franchini, E., C.J. Brito, and G.G. Artioli (2012). Weight loss in combat sports: physiological, psychological and performance effects. J. Int. Soc. Sports Nutr. 9:52-57.
He, F.J., N.D. Markandu, G.A. Sagnella, and G..A MacGregor (2001). Effect of salt intake on renal excretion of water in humans. Hypertension 38:317-320.
Hillemeier, C. (1995). An overview of the effects of dietary fiber on gastrointestinal transit. Pediatrics 96:997-999.
Holte, K., K.G. Nielson, J.L. Madsen, and H. Kehlet (2004). Physiologic effects of bowel preparation. Dis. Colon. Rectum 47:1397-1402.
Ivy, J.L., H.W. Goforth, B.M. Damon, T.R. McCauley, E.C. Parsons, and T.B. Price (2002). Early post exercise muscle glycogen recovery is enhanced with a carbohydrate-protein supplement. J. Appl. Physiol. 93:1337-1344.
James, L.J., and S.M. Shirreffs (2013). Fluid and electrolyte balance during 24-hour fluid and/or energy restriction. Int. J. Sport Nutr. Exerc. Metab. 23:545-553.
Kasper, A.M., S. Cocking, M. Cockayne, M. Barnard, J. Tench, L. Parker, J. McAndrew, C. Langan-Evans, G.L. Close, and J.P. Morton (2016). Carbohydrate mouth rinse and caffeine improves high-intensity interval running capacity when carbohydrate restricted. Eur. J. Sport Sci. 16:560-568.
Lambert, C.P., M.G. Flynn, J.B. Boone Jr, T.J. Michaud, and J. Rodriguez-Zayas (1991). Effects of carbohydrate feeding on multiple-bout resistance exercise. J. Strength Cond. Res. 5:192-197.
Lee, Y.Y., A. Erdogan, and S.S.C. Rao (2014). How to assess regional and whole gut transit time with wireless motility capsule. J. Neurogastroenterol. Motil. 20:265-270.
Lijoi, D., S. Ferrero, E Mistrangelo, I. Della Casa, M. Crosa, and V. Remorgida (2009). Bowel preparation before laparoscopic gynaecological surgery in benign conditions using a 1-week low fiber diet: a surgeon blind, randomized and controlled trial. Arch. Gynecol. Obstet. 280:713-718.
Mahan, L.K., and S. Escott-Stump (2008). Krause's Food and Nutrition Therapy, Saunders/Elsevier St. Louis.
Maughan, R., J. Leiper, and S. Shirreffs (1996). Restoration of fluid balance after exercise-induced dehydration: effects of food and fluid intake. Eur. J. Appl. Physiol. Occup. Physiol. 73:317-325.
Maughan, R.J., and J.B. Leiper (1999). Limitations to fluid replacement during exercise. Can. J. Appl. Physiol. 24:173-187.
Monro, J.A. (2000). Faecal bulking index: A physiological basis for dietary management of bulk in the distal colon. Asia Pac. J. Clin. Nutr. 9:74-81.
Pilch, W., Z. Szygula, T. Palka, P. Pilch, T. Cison, S. Wiecha, and L. Tota (2014). Comparison of physiological reactions and physiological strain in healthy men under heat stress in dry and steam saunas. Biol. Sport. 31:145-149.
Pizza, F.X., M.G. Flynn, B.D. Duscha, J. Holden, and E. Kubitz (1995). A carbohydrate loading regimen improves high intensity, short duration exercise performance. Int. J. Sport. Nutr. 5:110-116.
Ray, M.L., M.W. Bryan, T.M. Ruden, S.M. Baier, R.L. Sharp, and D.S. King (1998). Effect of sodium in a rehydration beverage when consumed as a fluid or meal. J. Appl. Physiol. 85:1329-1336.
Reale, R., G. Slater, and L.M. Burke (2016). Acute weight loss strategies for combat sports and applications to Olympic success. Int. J. Sports. Physiol. Perf. 12:142-151.
Reale, R., G. Slater, and L.M. Burke (2017a). Individualised dietary strategies for Olympic combat sports: Acute weight loss, recovery and competition nutrition. Eur. J. Sports. Sci. 17:727-740.
Reale, R., G. Slater, I.C. Dunican, G.R. Cox, and L.M. Burke. (2017b). The effect of water loading on acute weight loss following fluid restriction in combat sports athletes. Int. J. Sport Nutr. Exerc. Metab. 28:1 -22.
Sawka, M.N., S.N. Cheuvront, and R. Carter (2005). Human water needs. Nutr. Rev. 63:S30-S39.
Sawyer, J.C., R.J. Wood, P.W. Davidson, S.M. Collins, T.D. Matthews, S.M. Gregory, and V.J. Paolone (2013). Effects of a short-term carbohydrate-restricted diet on strength and power performance. J. Strength Cond. Res. 27:2255-2262.
Shirreffs, S.M., and R.J. Maughan (1998). Volume repletion after exercise-induced volume depletion in humans: replacement of water and sodium losses. Am. J Physiol. 274:F868-F875.
Walsh, R.M., T.D. Noakes, J.A. Hawley, and S.C. Dennis (1994). Impaired high-intensity cycling performance time at low levels of dehydration. Int. J. Sports Med. 15:392-8.
Wu, K.L., C.K. Rayner, S.K. Chuah, K.W. Chiu, C.C. Lu, and Y.C, Chiu (2011). Impact of low-residue diet on bowel preparation for colonoscopy. Dis. Colon Rectum 54:107-112.








