OVARIAN HORMONES 101; HOW TO CONDUCT HIGH-QUALITY SPORT AND EXERCISE SCIENCE RESEARCH ON FEMALE ATHLETES
Published
May 2023
Author
Kirsty Elliott-Sale, PhD, Institute of Sport, Manchester Metropolitan University, UK
Topics

KEY POINTS
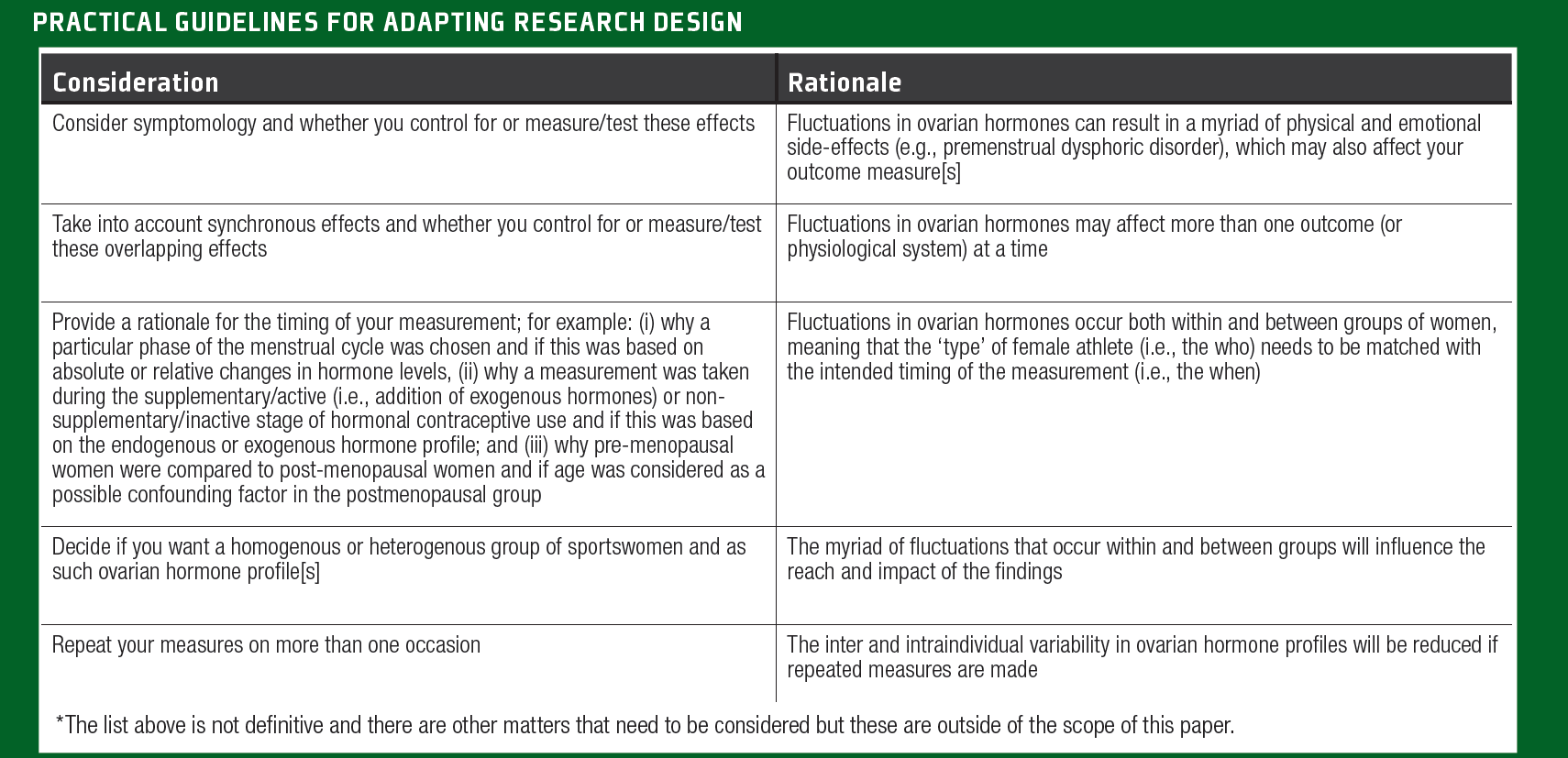
The rationale for including women as participants needs to be established before designing the study protocol to ensure that the appropriate participants are recruited, and the correct study design is employed.
The type of female athlete studied must be clearly defined and subsequently recruited to reduce between-participant variability in hormone status.
The exact method (estimated or verification) used to determine the ovarian hormonal profile studied must be clearly described and accurately determined to make certain that measurements were taken under the intended conditions.
Whenever possible, ‘gold-standard’ methods must be employed when undertaking female athlete-based research to increase the quantity of high- quality studies and strengthen our confidence in the findings and ability to translate them into evidence-based practice.
When it is not possible to use ‘gold-standard’ methods, the next best approach should be used and described as such to allow readers to interpret for themselves the true generalizability and impact of such findings
NOTE FROM THE AUTHOR
The article is written about cisgender women [i.e., someone who was assigned female at birth and identifies as a woman]. I have used the word female as an adjective [i.e., characteristic of girls, women, or the female sex: exhibiting femaleness] and the word woman as a noun [i.e., denoting an adult female human]. The terms sportswomen and female athletes are used interchangeably. When describing the work of others, I have adopted the language used by the authors themselves to describe their own work.
INTRODUCTION
Although almost half (49.7%) of the world’s population are women (United Nations, 2022), women are globally underrepresented in almost every aspect of professional sport: participation; scholarships; earnings; viewing figures; revenue; investment; coaching staff, sponsorship; prize money; marketing power; and social media presence (Statista, 2020). The same is true for sport and exercise science research; just 6% of studies published between 2014 and 2020 included females only, compared with 63% that included both sexes and 31% that included males only (Cowley et al., 2021). This is despite a 22-fold increase in participation rates for sportswomen in the Olympic Summer Games, from 2% in 1900 to 48.7% in the 2020 – contested in the 2021 Olympiad. Moreover, Cowley et al. (2021) conducted their audit on the basis of sex, using the following terms 'female', 'male', 'women', 'men', 'girls', 'boys', and not on athlete calibre; as such the representation of world-class and elite sportswomen (Tiers 4 and 5) in sport and exercise science research would likely be significantly less than in active women (Tiers 0-3; McKay et al., 2022). These statistics should make us ask: why have female athletes been marginalized in sport and exercise science research? There is no definitive answer to this question as individual researchers will have had their own reasons for not including sportswomen as participants in their studies. Rather than focusing on the probable reasons that sportswomen have largely been excluded from sport and exercise science research, a more constructive approach is to consider: WHY should we study female athletes? This Sport Science Exchange (SSE) article will address the ovarian hormone considerations needed for the inclusion of women as participants in sport and exercise science research.
REASONS FOR STUDYING FEMALE ATHLETES
There are many reasons for studying female athletes as part of sport and exercise science, and researchers should establish their own motives before undertaking research using sportswomen as participants. For example, sportswomen may be included on the basis of:
- Equality, diversity, and inclusivity - to make research findings more generalizable. Hagstrom et al. (2021) have called for researchers to include both male and female participants in similar numbers whenever possible and to always undertake sex disaggregation of their data so that data is generated for more than just 50% of the population.
- Logistics - to aid with recruitment and sample size when not studying sex-specific outcomes.
- Novelty - although just because someone hasn’t done it before, doesn’t always make it a good idea!
- The research question - the investigation of a potential or given female-specific consideration, which is usually grounded in a perceived (i.e., hasn’t been investigated before and is therefore at this time theoretical) or actual (i.e., has been noted before and warrants further investigation) biopsychosocial pathway.
In the case of the current paper, researchers might question how estrogen and progesterone affect a woman’s physiological, psychological, and social factors within a sport and exercise science context. In this instance, the next logical question is: Which women [WHO] should we study?
WHICH TYPES OF FEMALE ATHLETES WE SHOULD STUDY?
Whilst we can divide the sexes into males and females, females need to be further classified based on their sex hormone profile (Hackney & Elliott-Sale, 2021). As such, from an ovarian hormone perspective (i.e., the focus of the current paper) not all women are the same. It is a common misconception that all sportswomen have a menstrual cycle and should adopt a menstrual cycle phase-based approach to their training, diet, recovery, etc. From puberty to menopause, female athletes experience acute and chronic changes in ovarian hormones, with and without external influence, for example:
- The menstrual cycle [acute model] - daily and weekly changes in endogenous estrogen and progesterone levels, which repeat on an almost monthly basis.
- Hormonal contraceptives [acute and chronic model depending on the type of hormonal contraceptive used] - daily, weekly, and yearly changes in endogenous estrogen and progesterone levels, caused by the administration of exogenous estrogen and progestins.
- Pregnancy [chronic model] – weekly, monthly, and trimester- based changes in endogenous oestrogen and progesterone levels, resulting in supraphysiological levels of endogenous estrogen and progesterone.
- Menstrual dysfunction [acute and chronic model depending on the type of menstrual dysfunction experienced] – perturbation of the menstrual cycle, resulting in altered concentrations of endogenous estrogen and progesterone.
- Menopause [chronic model] –the complete cessation of the menstrual cycle.
As such, the who also influences the when: WHEN should we study female athletes
WHEN SHOULD WE STUDY FEMALE ATHLETES?
We can study female athletes across the lifespan or, for example, at/ under different:
- Phases of the menstrual cycle.
- Timepoints of hormonal contraceptive usage.
- Trimester of pregnancy.
- Stages of menopause.
- Menstrual dysfunction conditions.
Therefore, researchers should consider which type of female athletes should be the subject of their study and when/how often they should test them. Given the diversity of ovarian hormone profiles that sportswomen can experience during their lifetime, we should consider: HOW will we establish their ovarian hormonal profiles?
WAYS TO ESTABLISH OVARIAN HORMONE PROFILES
There are a number of ways that we can establish this, which range from inexpensive to expensive, non-invasive to invasive, and undemanding to burdensome measures, such as:
- Questionnaires (all ovarian hormone profiles) – asking for self- reported characteristics, knowledge, experiences, and opinions.
- Basal body temperature (menstrual cycle only) – charting average basal body temperatures over the length of a menstrual cycle to determine if ovulation has occurred (i.e., a temperature increase of ~0.3 – 0.6oC).
- Tracking bleeding and discharge patterns (menstrual cycles only) – noting the length and heaviness of bleeding during menstruation and the presence of a milky, white, vaginal discharge around the time of ovulation.
- Urine, saliva, and/or blood samples (all ovarian hormone profiles) – for the biochemical determination of estrogen and progesterone levels.
Given the paucity of research on female athletes, it can be difficult for researchers to determine how best to conduct research on female athletes. As such, researchers may ask: WHERE can we get credible information/advice on including female athletes in sport and exercise science research?
SOURCES OF CREDIBLE INFORMATION ON FEMALE ATHLETES
As female athlete research is such an underdeveloped area, it can be difficult for researchers and practitioners to have: (i) awareness of the current issues related to female athletes; (ii) knowledge and understanding of female-specific topics (especially female endocrinology); and (iii) the ability to correctly navigate the research evidence, especially as there is a lack of high-quality data in this area. Two recent sister systematic reviews and meta-analyses, on the effects of menstrual cycle phase and oral contraceptive use on athletic performance (Elliott-Sale et al., 2021; McNulty et al., 2021), showed that only 8% and 17% of the included studies were rated as high- quality, meaning that the majority of work in these areas was rated as very low, low, and moderate quality, therefore limiting our confidence in these findings. Moreover, several recent audits (Kuikman et al., 2022; Smith et al., 2022a,b) on the representation of female athletes in sports science and sports medicine research have shown a scarcity of high-quality female-specific datasets when assessed using a standardised audit tool and tiered ranking system (Smith et al., 2022c), which evaluates study quality based on participant classification and methodological control. As such, researchers and practitioners need to be critical of previous studies and judge publications on the directness and precision of the research design, for example, the clarity of reporting (e.g., how the female participants were defined based on their hormonal status) and robustness of research design (e.g., whether the ovarian hormone status was assumed, estimated, or verified). These domains should, of course, be considered alongside the other metrics associated with a high-quality approach (e.g., risk of bias, consistency, and evidence of publication bias). This leads us to the final consideration: WHAT measures/approaches should we take to increase the rigor and robustness of research on female athletes? This SSE article aims to provide guidance on how to conduct high- quality sport and exercise science research on female athletes through an ovarian hormone lens
PRACTICAL GUIDELINES FOR RECRUITING FEMALE PARTICIPANTS
Menstrual categorization systems are a useful tool for making an initial assessment of ovarian hormonal status in female athletes (Elliott-Sale et al., 2021); an exemplar is available in Figure 1 on page 7. These systems should be refined and adapted based on the type of female athletes intended for study.
Eumenorrheic Female Athletes
Definition. There are a number of criteria that need to be fulfilled before female athletes can be defined as eumenorrheic:
- Menstrual cycle lengths ≥ 21 days and ≤ 35 days.
- Ten or more consecutive periods per year.
- Evidence of a surge in luteinizing hormone [denoting ovulation].
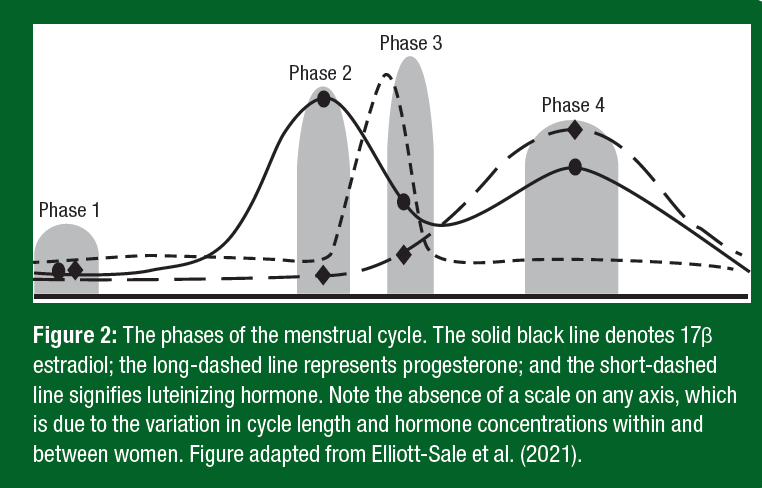
- Correct hormonal profile (Figure 2).
- Phase 1 – low estrogen and progesterone levels, indicated by the onset of bleeding.
- Phase 2 – estrogen levels higher than during phases 1, 3, and 4, and progesterone levels higher than phase 1 but lower than 6.4 nmol·L−1, which typically occurs in the 14–26 hours prior to ovulation and the luteinizing hormone surge.
- Phase 3 – estrogen levels higher than phase 1 but lower than phases 2 and 4, and progesterone levels higher than phase 1 but lower than 6.4 nmol·L−1, indicated by a positive urinary ovulation result, and lasts 24–36 hours.
- Phase 4 – estrogen levels higher than phases 1 and 3 but lower than phase 2 and progesterone levels >16 nmol·L−1to exclude luteal phase deficiency (Janse de Jonge et al., 2019), typically occurs seven days after ovulation has been confirmed.
- No hormonal contraceptive use within the last three months prior to recruitment.
How to establish this profile – practical implications for researchers. In order to establish eumenorrhea:
- Exclude female athletes who use hormonal contraceptives or have used them in the three months prior to recruitment.
- Exclude female athletes with known menstrual irregularities.
- Upon recruitment, determine typical cycle length by counting the number of days from the first day of menstruation to the day before the next onset of menstruation (must be ≥ 21 days and ≤ 35 days).
- Track cycle length and ovulation* over two or three cycles prior to the experimental stage of the study – if ovulation has not been confirmed then these female athletes should be excluded.
- Take a phase 4 blood sample for the determination of progesterone; this will likely be analysed once the experimental/ data collection part of the study is over, meaning that this information may be used for retrospective exclusion if luteal phase deficiency is evident.
- If possible, take a blood sample at each of the four phases of the menstrual cycle, for the determination of estrogen and progesterone, to verify (again probably retrospectively) each phase.
*Ovulation can be established by using the protocol outlined by O’Donnell, McCluskey & Stellingwerff (2022).
Naturally Menstruating Female Athletes
Definition. When all of the criteria for eumenorrhea cannot be established, the term naturally menstruating should be used to describe female athletes who, menstruate regularly (cycle length between 21 and 35 days), do not use hormonal contraceptives, and do not have any obvious/diagnosed menstrual irregularities (see section below). If ovulation has been confirmed, then these participants can be described as naturally menstruating and ovulating female athletes/participants.
How to establish this profile – practical implications for researchers. In order to recruit naturally menstruating female athletes:
- Exclude female athletes who use hormonal contraceptives or have used them in the three months prior to recruitment;
- Exclude female athletes with known menstrual irregularities;
- Upon recruitment, determine typical cycle length by counting the number of days from the first day of menstruation to the day before the next onset of menstruation (must be ≥ 21 days and ≤ 35 days);
- Ideally, track cycle length and ovulation (as described above) over two or three cycles prior to the experimental stage of the study – if ovulation is confirmed then these female athletes can be described as naturally menstruating and ovulating female athletes/participants.
Female Athletes with Menstrual Irregularities
Luteal Phase Deficiency. Definition. Cycles with less than 16 nmol·L−1of progesterone, when a single Phase 4 (see above) progesterone measurement is taken, are considered to be luteal phase deficient. Under these circumstances, the female athlete can still menstruate on a regular basis (i.e., have a 21-35 day cycle length). This is a “hidden” menstrual dysfunction, as without blood sample analysis the female athlete would not be aware of it (i.e., there is no obvious physical indicator that the phase 4 peak in progesterone has not occurred).
How to establish this profile – practical implications for researchers. In order to establish this condition:
- Exclude female athletes who use hormonal contraceptives or have used them in the three months prior to recruitment.
- Exclude female athletes with known menstrual irregularities.
- Upon recruitment determine typical cycle length, by counting the number of days from the first day of menstruation to the day before the next onset of menstruation (must be ≥ 21 days and ≤ 35 days).
- Establish ovulation (as described above) so that phase 4 can be predicted (i.e., seven days post ovulation).
- Take a phase 4 blood sample for the determination of progesterone; this will need to be analysed before the experimental stage of the study – female athletes with less than 16 nmol·L−1of progesterone can be described as luteal phase deficient.
Anovulatory Cycles. Definition. Cycles in which ovulation does not occur are termed anovulatory cycles. Under these circumstances, the female athlete can still menstruate on a regular basis (i.e., have a 21-35 day cycle length). This is a somewhat “hidden” menstrual dysfunction, as without using an ovulation detection kit, having a blood sample analysed, charting basal body temperature across the cycle, or noting vaginal discharges (which can be difficult to interpret) the female athlete would not necessarily be aware of it.
How to establish this profile – practical implications for researchers. In order to establish this condition:
- Exclude female athletes who use hormonal contraceptives or have used them in the three months prior to recruitment.
- Exclude female athletes with known menstrual irregularities.
- Upon recruitment determine typical cycle length, by counting the number of days from the first day of menstruation to the day before the next onset of menstruation (must be ≥ 21 days and ≤ 35 days).
- Track cycle length and ovulation (as described above) over two or three cycles prior to the experimental stage of the study – if ovulation is not confirmed then these female athletes can be described as anovulatory female athletes/participants.
In the case of the menstrual cycle-based research, we must not predict menstrual cycle phases based on bleeding patterns alone, either by counting days between menses or using current technologies such as phone apps, as menstruation alone does not determine a eumenorrheic menstrual cycle (i.e., female athletes with anovulatory and luteal phase deficient cycles – two types of menstrual irregularities - still experience menstruation).
Secondary Amenorrhea. Definition. The absence of ≥ 3 consecutive periods in non-pregnant women with past menses, is termed secondary amenorrhea. This is an “obvious” menstrual dysfunction, as the female athlete is aware of the cessation of menses.
How to establish this profile – practical implications for researchers. In order to establish this condition:
- Exclude female athletes who use hormonal contraceptives or have used them in the three months prior to recruitment.
- Exclude pregnant female athletes.
- Upon recruitment determine when menstruation last occurred – if menstruation did not occur within the last three months prior to recruitment, then these female athletes can be described as having secondary amenorrhea.
These are just three types of common menstrual irregularities experienced by female athletes, there are many others, which are outside of the scope of this paper.
Hormonal Contraceptive Using Female Athletes
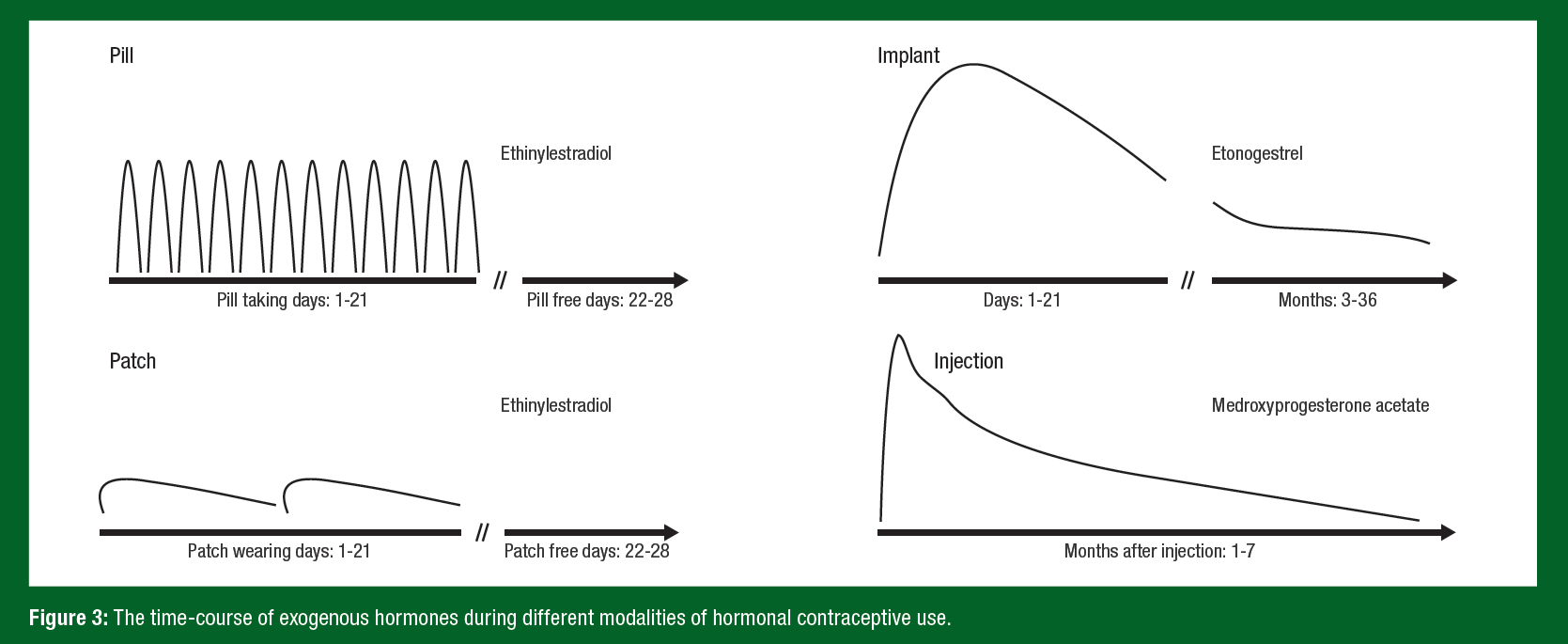
Definition. There are many types of hormonal contraceptives; for a comprehensive review see Elliott-Sale & Hicks (2018). In brief, hormonal contraceptives are agents capable of influencing the endogenous hormonal environment, through exogenous supplementation with either synthetic estrogen and progestin (i.e., combined) or progestin-only. They can be delivered via many modalities: oral administration (i.e., pills), subcutaneous injection, transdermal patches, and vaginal insertion (i.e., rings and t-shaped plastic devices). They prevent pregnancy by discontinuing ovulation, forming a thicker layer of cervical mucus that makes it difficult for sperm to reach the uterus, and affecting the uterine lining making it more difficult for an egg to attach. As such, female athletes who use hormonal contraceptives have significantly different hormonal profiles than either eumenorrheic female athletes or those with menstrual dysfunction. The profile of exogenous estrogen and/or progestin will differ based on the modality of administration (examples are shown in Figure 3), while the endogenous profiles will remain largely downregulated (i.e., without the cyclical variations – peaks and nadirs - seen in a eumenorrheic profile).
How to establish this profile – practical implications for researchers. In order to establish this group:
- Recruit participants that have been using their hormonal contraceptive for at least three months prior to recruitment.
Report the mode of administration (e.g., pill, implant, injection, intrauterine system, vaginal ring, transdermal patch), formulation (e.g., mono, bi or triphasic; combined or progesterone-only; names and concentration of exogenous hormones), and status (e.g., pill taking versus pill-free days, patch wearing versus patch-free days, how many days/months post-injection/implant).
Pregnant Female Athletes
Definition: Pregnancy typically lasts 40 weeks and is broken down into trimesters: trimester one is the first 13 weeks of pregnancy, trimester two is between weeks 14 and 27, and trimester three is from 27 weeks onwards. During this time, estrogen and progesterone levels steadily increase.
How to establish this profile – practical implications for researchers. In order to establish this group:
- Confirm pregnancy using a urinary pregnancy test kit or blood sample
- Determine gestation (i.e., the length of time, in days or weeks, that a baby is in the uterus) by ascertaining when menstruation last occurred.
- If known, state singleton or multiple pregnancy.
- If possible, take a blood sample at the time of measurement, to establish the exact hormonal milieu.
Menopausal Female Athletes
Definition: The transition from pre- to post-menopausal is difficult to describe and quantify. In the absence of hormonal contraceptive use, pregnancy, and menstrual dysfunction, women will transition, during menopause, from a menstrual cycle to a secondary amenorrhea profile. The peri-menopausal phase is characterised by lower estrogen levels than during the menstrual cycle and sporadic amenorrhea (Harlow et al., 2012). Post-menopause is defined as the time after which a woman has experienced 12 consecutive months of amenorrhea and is characterised by < 118 pmol∙L−1of estrogen, < 4.4 nmol∙L−1of progesterone and follicle stimulating-hormone > 25 IU∙L−1(Harlow et al., 2012).
How to establish this profile – practical implications for researchers. In order to establish this group:
- Exclude female athletes who use hormonal contraceptives or have used them in the three months prior to recruitment.
- Exclude female athletes with known menstrual irregularities.
- Exclude pregnant female athletes.
- Upon recruitment determine typical cycle length, by counting the number of days from the first day of menstruation to the day before the next onset of menstruation – short (< 21 days), long (> 35 days) and unpredictable menstrual cycle lengths are indicative of perimenopause.
- Track cycle length and ovulation* over two or three cycles prior to the experimental stage of the study – in addition to atypical variation in cycle length, anovulatory cycles are common during perimenopause.
- If possible, take a blood sample at the time of measurement, to establish the exact hormonal milieu – a peri-menopausal profile will have lower estrogen levels than during an eumenorrheic cycle and post-menopause oestrogen levels will be < 118 pmol∙L−1.
- Exclude female athletes using hormone replacement therapy, unless part of your research question, as hormone replacement therapy alters the endogenous hormonal milieu.
- If interested in the effects of hormone replacement therapy state the type and formulation used (e.g., tablets, skin patches, gels, implants, vaginal creams, pessaries or rings; combined
or estrogen-only; cyclical or continuous) and the length of time used prior to recruitment (this should be at least three months prior to recruitment).
There are other types of ovarian hormone profiles, which are outside of the scope of this paper. This paper represents the most common type of sportswomen studied in sport and exercise science.
SUMMARY
There is a lack of high-quality, female-specific data in sport and exercise science, which is hampering our ability to provide robust evidence-based guidelines to female athletes. In order to address this gap in knowledge and practice, researchers need to consider the ovarian hormone profiles that female athletes experience during their athletic careers and how these profiles affect the recruitment and design elements of sport and exercise science-related studies. As such, researchers need to be knowledgeable about female-specific endocrinology and have a rationale for the inclusion of sportswomen prior to deploying female athletes as participants in their studies. This will mean that the necessary adaptations are made to the research design, resulting in robust, meaningful datasets.
The views expressed in this article are those of the author and do not necessarily reflect the position or policy of PepsiCo, Inc.
REFERENCES
Statista DossierPlus on money in women's sport and the gender pay gap (2020). Available at https://www.statista.com/study/81865/money-in-women-s-sport/
Cowley, E.S., A.A. Olenick, K.L. McNulty, and E.Z. Ross (2021). “Invisible sportswomen”: The sex data gap in sport and exercise science research, Women Sport Phys. Activ. J. 29:146-151.
Elliott-Sale, K.J, and K. Hicks (2018). Hormonal-Based Contraception and the Exercising Female. In J. Forsyth, & C-M. Roberts (Eds.), The Exercising Female: Science and Its Application (Routledge Research in Sport and Exercise Science). Taylor & Francis.
Elliott-Sale, K.J., K.L. McNulty, P. Ansdell, S. Goodall, K.M. Hicks, K. Thomas, P.A. Swinton, and E. Dolan (2020). The effects of oral contraceptives on exercise performance in women: a systematic Review and meta-analysis. Sports Med. 50:1785-1812.
Elliott-Sale, K.J., C.L. Minahan, X.A.K. Janse de Jonge, K.E. Ackerman, S. Sipilä, N.W. Constantini, C.M. Lebrun, and A.C. Hackney (2021). Methodological considerations for studies in sport and exercise science with women as participants: A working guide for standards of practice for research on women. Sports Med. 51:843-861.
Elliott-Sale, K.J., K.L. McNulty, and C.L. Minahan (2022). Available at https://twitter.com/ ElliottSale/status/1497165205314232320).
Hackney, A.C., and K.J. Elliott-Sale (2021). Exercise Endocrinology: What Comes Next?.
Endocrines 2:167-170.
Hagstrom, A.D., N. Yuwono, K. Warton, and C.E. Ford (2021). Sex bias in cohorts included in sports medicine research. Sports Med. 51:1799-1804.
Harlow, S.D., M. Gass, J.E. Hall, R. Lobo, P. Maki, R.W. Rebar, S. Sherman, P.M. Sluss, and
T.J. de Villiers (2012). STRAW + 10 collaborative group. executive summary of the stages of reproductive aging workshop + 10: Addressing the unfinished agenda of staging reproductive aging. J. Clin. Endocrinol. Metab. 97:1159–1168.
Janse de Jonge X.A.K., B. Thompson, and A. Han (2019). Methodological recommendations for menstrual cycle research in sports and exercise. Med. Sci. Sports Exerc. 51:2610– 2617.
Kuikman, M.A., E.S. Smith, A.K.A. McKay, K.E. Ackerman, R. Harris, K.J. Elliott-Sale, T. Stellingwerff, and L.M. Burke (2022). Fuelling the female athlete: Auditing her representation in studies of acute carbohydrate intake for exercise. Med. Sci. Sports Exerc. Online ahead of print.
McKay, A.K.A., T. Stellingwerff, E.S. Smith, D.T. Martin, I. Mujika, V.L. Goosey-Tolfrey, J. Sheppard, and L.M. Burke (2022). Defining training and performance caliber: A participant classification framework. Int. J. Sports Physiol. Perform. 17:317-331.
McNulty, K.L., K.J. Elliott-Sale, E. Dolan, P.A. Swinton, P. Ansdell, S. Goodall, K. Thomas, and
K.M. Hicks (2020). The effects of menstrual cycle phase on exercise performance in eumenorrheic women: A systematic review and meta-analysis. Sports Med. 50:1813- 1827.
O’Donnell, J., P. McCluskey, and T. Stellingwerff (2022). Available at http://www.csipacific. ca/wp-content/uploads/2022/09/CSI-Pacific-Ovuation-Protocol-20220921.pdf
Smith, E.S., A.K.A. McKay, M. Kuikman, K.E. Ackerman, R. Harris, K.J. Elliott-Sale, T. Stellingwerff, and L.M. Burke (2022a). Auditing the representation of female versus male athletes in sports science and sports medicine research: Evidence-based performance supplements. Nutrients 14:953.
Smith, E.S., A.K.A. McKay, M. Kuikman, K.E. Ackerman, R. Harris, K.J. Elliott-Sale, T. Stellingwerff, and L.M. Burke (2022b). Managing female athlete health: auditing the representation of female versus male participants among research in supplements to manage diagnosed micronutrient issues. Nutrients 14:3372.
Smith, E.S., A.K.A. McKay, K.E. Ackerman, R. Harris, K.J. Elliott-Sale, T. Stellingwerff, and
L.M. Burke (2022c). Methodology review: A protocol to audit the representation of female athletes in sports science and sports medicine research. Int. J. Sport Nutr. Exerc. Metab. 32:114-127.
United Nations 2022 Revision of World Population Prospects. Available at https://population. un.org/wpp/
.jpg?sfvrsn=71e2ba23_0)








