Beyond sport: Hydration and Body Cooling Considerations to Prevent Heat-Related Injury and Improve Productivity - Part 2
Published
June 2025
Author
Margaret C Morrissey-Basler, PhD, Gabrielle J Brewer, PhD, Douglas J Casa, PhD

KEY POINTS
- To effectively manage heat exposure, a comprehensive approach should be taken that includes strategies such as a written heat stress management plan, heat acclimatization protocols, worker education, environmental monitoring, emergency response procedures and interventions focused on hydration and body cooling.
- Workers frequently begin work in a hypohydrated state and during work dehydration is prevalent due to fluid loss through sweating, limited fluid intake and restroom accessibility.
- Current research indicates that hydration interventions such as providing water, water-electrolyte solutions or implementing “Water, Rest, Shade” programs reduce the risk of dehydration, productivity decrements and acute kidney injury.
- The National Institute for Occupational Safety and Health (NIOSH) recommends drinking 24-32 ounces (710-950 mL) of water per hour during heat exposure, with electrolytes added when work in the heat exceeds two hours. These recommendations were developed from data from healthy, young male workers.
- Low-cost, feasible body cooling strategies such as shade, electric fans, body cooling towels and gear, and cooling vests should be considered in the workplace. To maximize effectiveness, body cooling methods should cover the largest possible body surface area, maintain a low temperature and remain in contact with the worker for an extended duration.
INTRODUCTION
The Sport Science Exchange (SSE) article, “Beyond Sport: Acute and Long-Term Health Issues and Considerations for Workers in a Warmer World” described the acute and chronic impact of heat exposure on workers’ health, safety and productivity. Health impacts range from discomfort, fatigue, heat exhaustion, muscle damage and acute kidney injury to life-threatening conditions such as exertional heat stroke, chronic kidney disease and cardiac mortality (Casa et al., 2015; Crowe et al., 2023; WHO, 1969). Excessive occupational heat exposure can also negatively impact physical work capacity and productivity outcomes, which negatively affects economic growth (Borg et al., 2021; Flouris et al., 2018; Foster et al., 2021). Considering the significant effects of heat on workers, implementing evidence-based prevention strategies is essential to reduce associated risks and performance decrements.
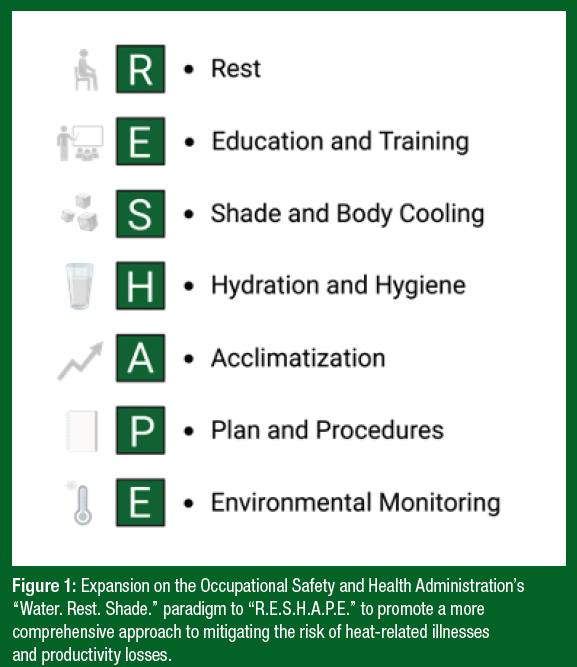
In 2011, the Occupational Safety and Health Administration (OSHA) introduced a campaign called, “Water. Rest. Shade.” (WRS), which was created to promote three key practical prevention strategies to help reduce risk of occupational heat-related illnesses (OSHA, 2011). The implementation of these strategies is essential, however, additional measures such as a written heat stress management plan, heat acclimatization, education, active body cooling, personal protective equipment (PPE), hygiene, environmental monitoring and emergency response procedures should also be considered to enhance the protection of vulnerable workers and fully utilize all available resources (Morrissey et al., 2021a; Morris et al., 2019). Health and safety professionals and employers should consider broadening OSHA’s WRS paradigm to "R.E.S.H.A.P.E." to promote a more comprehensive approach to mitigating the risk of heat-related illnesses and productivity losses associated with heat exposure (Figure 1). In response to the growing focus and inquiries surrounding hydration and body cooling practices in the workplace, this SSE article will comprehensively explore these two preventive strategies.
HYDRATION
Sweat evaporation is the primary mechanism for heat dissipation when relative humidity is low. When sweat losses exceed fluid intake, and no fluid replacement strategy is in place, workers experience a body water deficit called hypohydration through the process of dehydration, which is the process by which body water is lost within the body (Cheuvront et al., 2003). Euhydration refers to normal or “optimal” body water content (Cheuvront et al., 2003). Hypohydration and dehydration are prevalent in both heat-exposed and non-heat-exposed working populations (Flouris et al., 2018). Recent studies indicate that 15-100% of workers arrive at their worksite hypohydrated and do not adequately replace fluids during work, especially when working in a hot environment (Brake & Bates, 2003; Kenefick & Sawka, 2007; Nerbass et al., 2019; Piil et al., 2018; Wagoner et al., 2020; Wesseling et al., 2016). Flouris et al. (2018) reported that individuals working a single shift in a hot environment had a 14.5% increase in urine specific gravity, a marker of dehydration, compared with those who worked a shift in thermoneutral conditions. Work environments, compared to other settings such as sports, provide additional challenges that limit workers’ ability to adequately replace lost fluids (Morrissey et al., 2021b). For example, workers are often required to wear PPE during work, which can both limit their ability to consume fluids throughout the workday and limit sweat evaporation. Optimizing rehydration by matching sweat rate can be very challenging in occupational settings, especially when opportunities to drink are limited or when consuming large amounts of fluid causes gastrointestinal discomfort (Hew-Butler et al., 2019). Moreover, many work environments have limited access to clean potable drinking water and restrooms. Female workers may be at greater risk of dehydration due to limited restroom access facilities for females (Venugopal et al., 2016). Unfortunately, females may limit their water intake to avoid the need to use restroom facilities (Morrissey-Basler et al., 2023). In remote work settings, there are extra challenges because fluid sources must be portable, remain cool and palatable, and made available through an entire work shift. It is critical for employers and managers to identify and execute methods to enhance fluid accessibility and availability during a work shift to allow for adequate fluid replacement in the heat (Adams et al., 2024; Armstrong et al., 2025; Stoecklin-Marois et al., 2013).
Physiological and Health Impacts
Dehydration in the absence of proper fluid replacement, especially in hot environments, can negatively impact worker physiology and well-being (Houser et al., 2021; Piil et al., 2018; Wegman et al., 2018). A decrease in total body water reduces blood volume, increases heart rate (HR) and decreases stroke volume to maintain cardiac output (Cheuvront et al., 2003). For example, Adams et al. (2014) reported that HR increased by an average of 3-5 beats/min for every 1% of body mass loss. Additionally, the rate at which HR recovers following intense exercise in the heat will be greatly diminished when dehydrated (Casa et al., 2010). Working in a dehydrated state can increase core temperature, decrease sweat rate and decrease skin blood flow at a given core temperature, exacerbating physiological strain (Casa, 1999). Body temperature also increases concomitantly with increasing dehydration, while performing physical activity in the heat. Studies have reported that body temperature increases ~0.25°C for every additional 1% body mass loss (Casa et al., 2010; Lopez et al., 2011). Moreover, a significant health consequence of performing physical work in the heat is the risk of acute kidney injury (AKI), which results from repeated episodes of hyperthermia, exposure to environmental agents (i.e., pesticides, heavy metals) and dehydration (Amorim & Schlader, 2025; Chapman et al., 2020, 2021). A study in Florida agriculture workers (n=192) reported that over 3 testing days, 53% of workers arrived at work hypohydrated and 81% were hypohydrated at the end of their shift. Many participants (33%) developed AKI on at least 1 of the 3 days (Mix et al., 2018). Similarly, the incidence of AKI in Guatemalan agriculture workers was 53%, 54%, and 51% in February, March, and April, respectively, with hypohydration being a major risk factor (Butler- Dawson et al., 2019).
Productivity Impacts
Increases in physiological strain induced by dehydration can also negatively affect physical work capacity and labor productivity (Adams et al., 2019; Morrissey et al., 2021b). Much of the research examining the impact of dehydration on work capacity has been performed in sport-related activities, reporting that exercise inducing a 2% body mass loss, paired with inadequate fluid intake, impairs endurance performance (Adams et al., 2018, 2019). In the occupational setting, Zimbabwean forest workers engaging in manual harvesting were examined across two different hydration conditions: 1) consumed 0.17 L of water every half hour to limit fluid intake (low fluid group), or 2) consumed 0.61 L of water every half hour to maintain euhydration (high fluid group) (Wästerlund et al., 2004). Each experimental condition lasted 4 days and in the low fluid group, participants harvested 12% less trees compared to the high fluid group. Similarly, Delgado- Cortez (2009) observed that 59% of sugarcane workers (13/22) who had the highest product output (6-8 tons) drank more than 6 L of fluid a day compared to workers who drank less and had smaller production output.
Water Consumption Interventions
To mitigate the adverse effects of dehydration on worker physiology, health and productivity, it is crucial to implement hydration strategies (Morrissey et al., 2021a). Multiple studies have examined the influence of hydration interventions on the incidence of hypohydration, health and productivity (Chapman et a., 2020; Chicas et al., 2022; Glaser et al., 2020; Ioannou et al., 2021a; Krisher et al., 2020; Wegman et al., 2018) (Table 1). Chapman et al. (2020) reported that a replacement of 100% of body weight loss during work in the heat with water consumption reduced creatinine clearance, a marker of AKI, by 16% compared to no fluid replacement. In a multi-country intervention, Ioannou et al. (2021a) implemented a hydration intervention of 750 mL of water every hour in workers from the agriculture industry in Qatar, construction industry in Qatar and construction industry in Spain. This hydration strategy reduced the prevalence of hypohydration by 54, 97 and 13%, respectively. They also reported that in all work environments, core temperature was significantly reduced, and productivity was unaffected (Ioannou et al., 2021a).
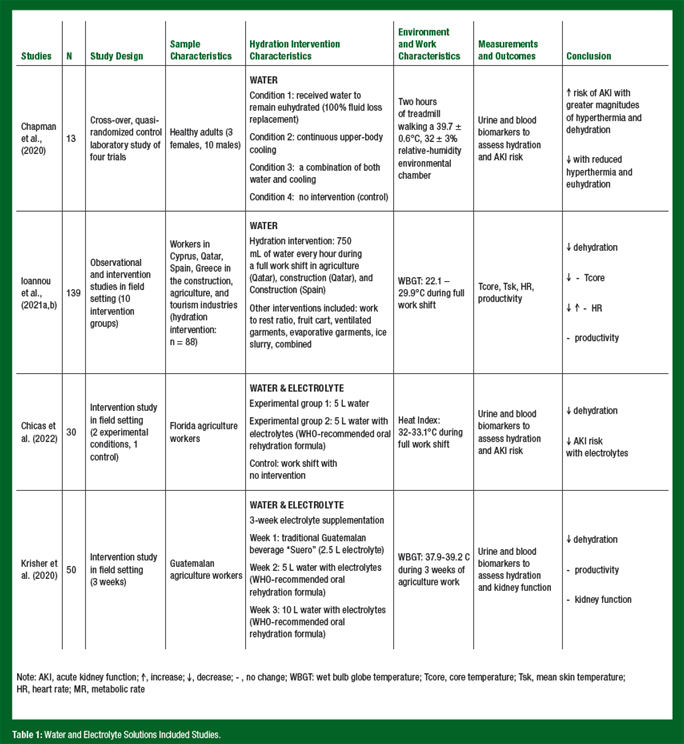
Electrolyte Solution Interventions
Several studies have examined hydration interventions that included electrolyte solutions (Chicas et al., 2022; Krisher et al., 2020). As dehydration during work is a direct result of increased sweat losses, it is important to note that electrolytes are also lost in sweat (Sawka & Montain, 2000). Body water contains electrolytes which aid in the movement of fluid between intra- and extracellular compartment and maintain membrane electrochemical potentials (Sawka & Montain, 2000). Electrolyte supplementation can also prevent hyponatremia in work conditions that allow for longer timeframes for fluid ingestion (Sawka & Montain, 2000). The impact of fluid and electrolyte supplementation in occupational settings has primarily focused on the risk of AKI and productivity outcomes in agriculture workers. A study in Florida agriculture workers (n=30) examined the influence of two hydration interventions during a single work shift in the heat compared to an observational workday control (control group): 1) 5 L of water (water group), or 2) 5 L of water with a glucose-electrolyte solution (glucose-electrolyte group) based on the World Health Organization (WHO) recommended oral rehydration formula (i.e., per 1 L, formula must contain: 13.5 g glucose, 2.9 g trisodium citrate dihydrate, 2.6 g sodium chloride and 1.5 g potassium chloride) (Chicas et al., 2022). Incidence of AKI post-work was 18% in the control condition, 23% in the water group and 0% in the glucose-electrolyte group. Similarly, Krisher et al. (2020) evaluated the impact of a 3-week electrolyte supplementation on hydration status, productivity and AKI in Guatelmalan agriculture workers (n=50) performing physically demanding work in the heat. Participants were provided with an electrolyte solution with the WHO-recommended oral rehydration formula (glucose-electrolyte solution) with 5 L of water and 10 L of water during week 2 and 3, respectively (Krisher et al. 2020). There was no electrolyte intervention during week 1, however, each worker was provided a traditional Guatelmalan beverage (“suero”), which was 2.5 L of electrolyte solution (electrolyte concentration not described) per day (Krisher et al., 2020). While productivity did not change across all three weeks, no participants were hypohydrated (<1.020 urine specific gravity) and kidney function was maintained throughout the intervention.
Water. Rest. Shade. Interventions
Hydration interventions have also been implemented as part of a “Water. Rest. Shade.” (WRS) program (OSHA, 2011). Wegman et al. (2018) examined whether the implementation of a WRS program would reduce biomarkers of kidney function during a single shift and across a portion of the harvest season in inland and coastland sugarcane workers. Participants were given a 3 L water backpack, a 40 L water thermos to refill, a mobile shaded tent and 10-15 min rest breaks every 1-1.5 hours (Wegman et al., 2018). Prior to the intervention, the mean decrease of estimated glomerular filtration rate (eGFR), a kidney function biomarker estimated using the Chronic Kidney Disease Epidemiology Collaboration creatinine equation (Levey et al., 2009), across a single work shift was -10.5 mL/min/1.73m2 compared to baseline. At the end of the 5-month harvest following the intervention, both groups (inland and coastland workers) had a reduction of only -3.4 mL/min/1.73m2 compared to baseline (Wegman et al., 2018). In sugarcane workers, Glaser et al. (2020) reported that greater access to water, electrolytes, rest and shade in Harvest 2 compared to a previous harvest (Harvest 1), decreased incident kidney injury rate and eGFR in the burned cane cutters group with self-reported larger water and electrolyte solution consumption intake in Harvest 2.
Hydration Recommendations
While there is no occupational standard to mandate hydration practices, the National Institute for Occupational Health and Safety (NIOSH) recommends drinking 24 to 32 ounces (710 to 950 mL) of water/hour when working in the heat (NIOSH, 2016). However, worksite, industry and individual characteristics should be considered when determining appropriate fluid recommendations. NIOSH also recommends consuming electrolytes if work duration exceeds 2 hours, however, there is no guidance on the amount or mixture of electrolytes to consume (NIOSH, 2016). In sport, electrolyte replacement is based on normative data on sweat rate and sweat composition in athletes (Baker et al., 2016). However, no such data exists for workers. Current research studies have utilized the WHO recommended oral rehydration formula (WHO, 2006) that is designed to treat diarrhea diseases and may not be appropriate for workers. It is also unclear whether electrolyte consumption in the heat should be limited in workers with hypertension or high sodium diets. In summary, more research is warranted to appropriately prescribe fluid and electrolyte solutions to working populations.
BODY COOLING
Body cooling has received significant attention as a preventive strategy as it has been shown to reduce physiological, cognitive and physical strain during work in the heat (Chicas et al., 2020; DeMartini et al., 2011; Morris et al., 2020; Morrissey et al., 2021a). Air conditioning is considered the most effective body cooling strategy; however, this solution is not sustainable due to its reliance on fossil fuels, contributions to greenhouse gases, the requirement for a power supply and high operational costs (Davis & Gertler, 2015; Abel et al., 2018; Girgis et al., 2016; Morris et al., 2020). Furthermore, it is not practical to install air conditioning in large factories or warehouses with frequent open-air exposure (e.g., loading docks). Workplaces require sustainable, low-cost body cooling solutions to ensure widespread adoption to effectively mitigate heat strain and enhance productivity (Morris et al., 2020; Morrissey-Basler et al., 2024). Shade has been included in several occupational heat stress standards for outdoor workers because it is cost-effective, accommodates multiple workers simultaneously and reduces worker exposure to solar radiation as a method of reducing heat strain (ANSI/ASSP, 2024; Morabito et al., 2020; NRDC, 2024). Few studies have examined the direct impact of shade on thermoregulation or productivity. One study did report a 6-fold increase in productivity if workers performed work under the shade (Morabito et al., 2020). However, several studies have examined the influence of solar radiation on thermoregulation during physical work (Ioannou et al., 2021b; Otani et al., 2019, 2021). For example, Ioannou et al. (2021b) performed four multi-country studies examining the impact of sun exposure on work physiology and cognition. The studies reported that workers experienced more frequent heat-related illnesses or strain symptoms, increased skin temperature, sweat rate, skin blood flow and heart rate. The cognitive assessments reported that attention and vigilance test outcomes were reduced by 45 and 67% during sun exposure compared to no sun exposure (Ioannou et al., 2021b). In a simulated occupational work environment in the heat, after the removal of the solar radiation lamp (i.e., “shade”), Morrissey-Basler et al. (2024) reported a 14% increase in the number of boxes lifted during a box lifting productivity activity. There are also studies that report a positive impact of shade within a WRS program (Glaser et al., 2020; Wegman et al., 2018).
There is also a growing interest in active cooling modalities in the workplace, including electric fans, specialized cooling garments, cooling vests, cooling towels and gear, and extremity cooling (Figure 2) (Kaufman et al., 2025; Morris et al., 2020; Morrissey et al., 2021a). Current literature suggests that these methods are effective by enhancing conductive heat transfer from the core to the skin or enhancing sweating efficiency, thereby reducing heat strain (Morris et al., 2020). An umbrella review reported, across 36 systematic reviews on occupational heat strain mitigation strategies, specialized cooling garments (i.e., air cooled, liquid cooled), fanning, mist fanning, shading and cold-water immersion were among the most effective strategies (Morris et al., 2020). Enhancing air movement through electric fan use has been proposed as an alternative or in conjunction with air conditioning as it can be transported and does not interfere with the normal operations of the workday (Hospers et al., 2020; Jay et al., 2015; Morris et al., 2019). However, it should be recognized that electric fan use can be detrimental in very hot and dry conditions and non-effective while wearing insulative PPE (Jay et al., 2015). Workers would benefit from using conductive heat transfer methods such as body cooling garments and vests during these conditions.
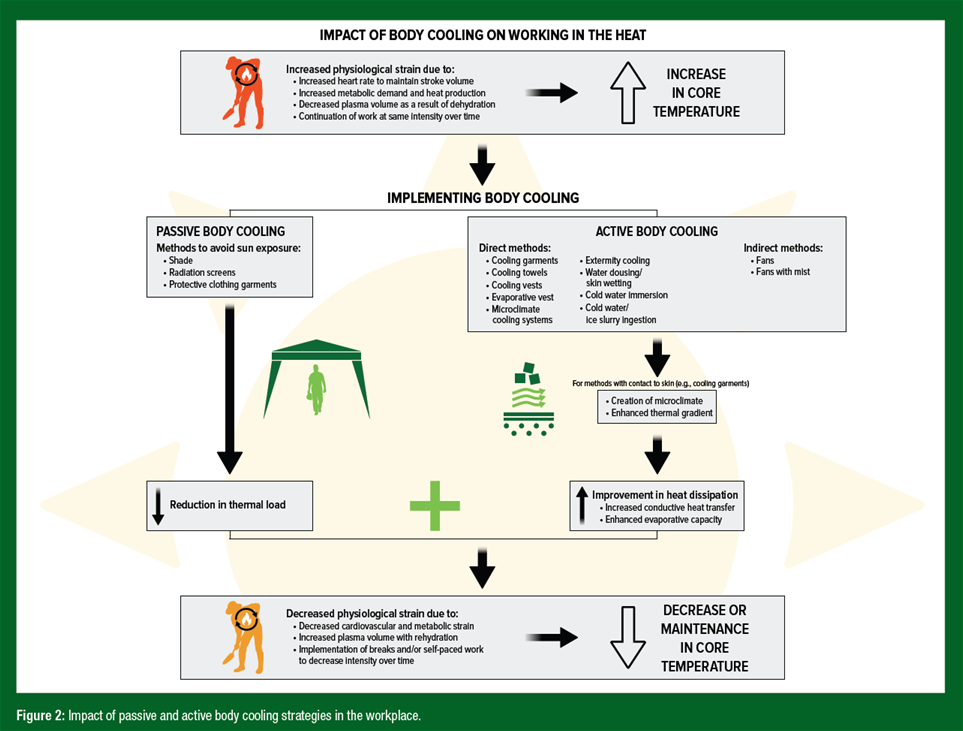
When selecting an appropriate body cooling strategy, workplaces must consider cost, sustainability and feasibility within their specific work conditions. Many work conditions do not have access to power or cannot remove their PPE, which poses a significant challenge for implementing many body cooling modalities (Morrissey et al., 2021a). Moreover, the effectiveness of each cooling method is influenced by several factors, including the body surface area exposed, the temperature of the cooling modality, and the duration of the cooling (Brearley, 2016; Bongers et al., 2017; Casa et al., 2007; DeMartini et al., 2011; Douzi et al., 2019). Multiple body cooling modalities or heat stress mitigation strategies should be considered to address these factors and optimize cooling. For instance, it has been shown that, during simulated occupational work in hot conditions, the use of active body cooling during rest breaks, cooling vests during physical activity, hydration and eliminating the radiant heat load led to greater reductions in physiological strain and enhanced box lifting performance compared to the control condition (Morrissey-Basler et al., 2024). In addition, it has been reported that combining a hydration strategy to maintain euhydration and water dousing during physical activity in the heat, had greater physiological benefits than water dousing or maintenance of euhydration alone (Benjamin et al., 2021). As previously noted, the specific body cooling methods implemented in work environments will vary based on factors such as available resources, the presence of other safety hazards, the duration and setting of rest breaks and the level of worker acceptance and engagement.
PRACTICAL APPLICATIONS
Implementing evidence-based prevention strategies is essential to reduce adverse health and productivity effects. For hydration and body cooling practices in the workplace, the following practical applications are proposed:
- To optimize fluid accessibility and availability, work environments must ensure workers have easy access to clean potable drinking water and restrooms, particularly for female workers.
- In remote work settings, fluid sources must be potable, cool, portable and available during the entire work shift.
- Hydration interventions such as water, water-electrolyte solution and Work. Rest. Shade. programs in the workplace reduce risk of dehydration and acute kidney injury.
- Current hydration recommendations recommend drinking 24 to 32 ounces (710 to 950 mL) of water an hour when working in the heat and recommended consumption of electrolytes when work duration exceeds 2 hours. These recommendations stem from data from healthy, young male workers. Data on female workers and workers with cardiovascular risk factors are needed.
- Workplaces require sustainable, low-cost body cooling solutions such as shade, electric fans, cooling vests and cooling gear.
- To maximize body cooling effectiveness, modalities should cover the largest possible body surface area, maintain a low temperature and remain in contact with the worker for an extended duration.
- Multiple body cooling or heat stress mitigation strategies should be implemented to receive the greatest reductions in physiological strain and improve productivity outcomes.
SUMMARY
Excessive occupational heat exposure adversely affects health, safety and productivity outcomes. To address these risks, implementing evidence-based prevention strategies is essential. Hydration and body cooling are among the most important prevention strategies to consider. Dehydration is common among workers due to fluid loss through sweating, limited access to fluids and limited access to restroom facilities. Current research indicates that hydration interventions such as providing water, water-electrolyte solutions or implementing Work. Rest. Shade. programs improve hydration status, productivity and kidney function. NIOSH recommends drinking 24 to 32 ounces (710 to 950 mL) of water per hour during heat exposure, with electrolytes added when work in the heat exceeds two hours. However, these recommendations are based on healthy, young males and may not support hydration needs for females or workers with cardiovascular risk factors. Similarly, low-cost body cooling strategies such as shade, electric fans, body cooling towels and gear, cooling vests and extremity cooling can reduce heat strain and enhance productivity. To maximize body cooling effectiveness, multiple strategies should be adopted, the largest possible body surface area should be covered and cooling modalities should maintain a low temperature for extended periods. Both body cooling and hydration interventions should be adapted to the specific work environment, accounting for factors such as resource accessibility and operational feasibility.
The views expressed are those of the authors and do not necessarily reflect the position or policy of PepsiCo, Inc.
REFERENCES
Abel, D.W., T. Holloway, M. Harkey, P. Meier, D. Ahl, V.S. Limaye, and J.A. Patz (2018). Air-quality-related health impacts from climate change and from adaptation of cooling demand for buildings in the eastern United States: An interdisciplinary modeling study. PLoS Med. 15:e1002599.
Adams, J.D., Y. Sekiguchi, H.-G. Suh, A.D. Seal, C.A. Sprong, T.W. Kirkland, and S.A. Kavouras (2018). Dehydration impairs cycling performance, independently of thirst: A blinded study. Med. Sci. Sports Exerc. 50:1697–1703.
Adams, J.D, D.M. Scott, N.A. Brand, H.G. Suh, A.D. Seal, B.P. McDermott, M.S. Ganio, and S.A. Kavouras (2019). Mild hypohydration impairs cycle ergometry performance in the heat: A blinded study. Scand. J. Med. Sci. Sports. 29:686–695.
Adams, W.M., E.M. Ferraro, R.A. Huggins, and D.J. Casa (2014). Influence of body mass loss on changes in heart rate during exercise in the heat: A systematic review. J. Strength Cond. Res. 28:2380–2389.
Adams, W.M., T. Anderson, M.E. Zaplatosch, S.N. Cheuvront, R.W. Kenefick, B.A. Yates, M.C. Morrissey-Basler, D. J. Casa, and L. Wideman (2024). Utility of body weight, urine color, and thirst perception (WUT) in determining hydration in young adults. Med. Sci. Sports Exerc. 56:2404–2412.
American National Standards Institute & American Society of Safety Professionals (ANSI/ ASSP) (2024). A10.50-2024: Heat stress management in construction and demolition operations (Digital ed.). https://store.assp.org
Amorim, F., and Z. Schlader (2025). The kidney under heat stress: A vulnerable state. Curr. Opin. Nephrol. Hyperten. 34:170–176.
Armstrong, L.E, R.L. Stearns, R.A. Huggins, Y. Sekiguchi, A.J. Mershon, and D.J. Casa (2025). Reference values for hydration biomarkers: Optimizing athletic performance and recovery. Open Acc. J. Sports Med. 16:31–50.
Baker, L.B., K.A. Barnes, M.L. Anderson, D.H. Passe, and J.R. Stofan (2016). Normative data for regional sweat sodium concentration and whole-body sweating rate in athletes. J. Sports Sci. 34:358–368.
Benjamin, C.L., Y. Sekiguchi, M.C. Morrissey, C.R. Butler, E.M. Filep, R.L. Stearns, and D.J. Casa (2021). The effects of hydration status and ice-water dousing on physiological and performance indices during a simulated soccer match in the heat. J. Sci. Med. Sport 24:723–728.
Bongers, C.C., W.G. Maria, T.E. Hopman, and T.M.H. Eijsvogels (2017). Cooling interventions for athletes: An overview of effectiveness, physiological mechanisms, and practical considerations. Temp. Multidisc. Biomed. J. 4:60–78.
Borg, M.A., J. Xiang, O. Anikeeva, D. Pisaniello, A. Hansen, K. Zander, K. Dear, M.R. Sim, and P. Bi (2021). Occupational heat stress and economic burden: A review of global evidence. Environ. Res. 195:110781.
Brake, D.J., and G.P. Bates (2003). Fluid losses and hydration status of industrial workers under thermal stress working extended shifts. Occup. Environ. Med. 60:90–96.
Brearley, M. (2016). Cooling methods to prevent heat-related illness in the workplace. Workplace Health Saf. 64:80.
Butler-Dawson, J., L. Krisher, H. Yoder, M.D., C. Sorensen, R.J. Johnson, C. Asensio, A. Cruz, E.C. Johnson, E.J. Carlton, L. Tenney, E.J. Asturias, and L.S. Newman (2019). Evaluation of heat stress and cumulative incidence of acute kidney injury in sugarcane workers in Guatemala. Int. Arch. Occup. Environ. Health. 92:977–990.
Casa, D.J. (1999). Exercise in the heat. I. Fundamentals of thermal physiology, performance implications, and dehydration. J. Athl. Train. 34:246–252.
Casa, D.J., B.P. McDermott, E.C. Lee, S.W. Yeargin, L.E. Armstrong, and C.M. Maresh (2007). Cold water immersion: The gold standard for exertional heatstroke treatment. Exerc. Sport Sci. Rev. 35:141–149.
Casa, D.J., R.L. Stearns, R.M. Lopez, M.S. Ganio, B.P. McDermott, S.W. Yeargin, L.M. Yamamoto, S.M. Mazerolle, M.W. Roti, L.E. Armstrong, and C.M. Maresh (2010). Influence of hydration on physiological function and performance during trail running in the heat. J. Athl. Train. 45:147–156.
Casa, D.J., J.K. DeMartini, M.F. Bergeron, D. Csillan, E.R. Eichner, R.M. Lopez, M.S. Ferrara, K.C. Miller, F. O'Connor, M.N. Sawka, and S.W. Yeargin. (2015). National Athletic Trainers’ Association position statement: Exertional heat illnesses. J. Athl. Train. 50:986–1000.
Chapman, C.L., B.D. Johnson, N.T. Vargas, D. Hostler, M.D. Parker, and Z.J. Schlader (2020). Both hyperthermia and dehydration during physical work in the heat contribute to the risk of acute kidney injury. J. Appl. Physiol. 128: 715–728.
Chapman, C.L., H.W. Hess, R.A.I. Lucas, J. Glaser, R. Saran, J. Bragg-Gresham, D.H. Wegman, E. Hansson, C.T. Minson, and Z.J. Schlader. (2021). Occupational heat exposure and the risk of chronic kidney disease of nontraditional origin in the United States. Am. J. Physiol. 321:R141–R151.
Cheuvront, S.N., R. Carter, and M.N. Sawka (2003). Fluid balance and endurance exercise performance. Curr. Sports Med. Rep. 2:202–208.
Chicas, R., N. Xiuhtecutli, N.E. Dickman, M.L. Scammell, K. Steenland, V.S. Hertzberg, and L. McCauley (2020). Cooling intervention studies among outdoor occupational groups: Aa review of the literature. Am. J. Indust. Med. 63:988–1007.
Chicas, R., J. Suarez, L. Elon, N. Xiuhtecutli, M.C. House, L. Berra, J.M. Sands, V. Hertzberg, and L. McCauley (2022). Hydration interventions among agricultural workers. J. Occup. Environ. Med. 64:e357–59.
Crowe, J., B. Knechtle, and D. Rojas-Valverde (2023). Editorial: Acute and long-term health issues of occupational exposure to heat and high physical loads. Front. Physiol. 14:1304229.
Davis, L.W., and P.J. Gertler (2015). Contribution of air conditioning adoption to future energy use under global warming. Proc. Nat. Acad. Sci. U.S.A. 112:5962-5967.
Delgado-Cortez, O. (2009). Heat stress assessment among workers in a Nicaraguan sugarcane farm. Global Health Action. 2:2069.
DeMartini, J.K., G.F. Ranalli, D.J. Casa, R.M. Lopez, M.S. Ganio, R.L. Stearns, B.P. McDermott, L.E. Armstrong, and C.M. Maresh (2011). Comparison of body cooling methods on physiological and perceptual measures of mildly hyperthermic athletes. J. Strength Cond. Res. 25:2065–2074.
Douzi, W., B. Dugué, L. Vinches, C. Al Sayed, S. Hallé, L. Bosquet, and O. Dupuy (2019). Cooling during exercise enhances performance, but the cooled body areas matter: A systematic review with meta-analyses. Scand. J. Med. Sci. Sports. 29:1660–1676.
Flouris, A.D., P.C. Dinas, L.G. Ioannou, L. Nybo, G. Havenith, G.P. Kenny, and T. Kjellstrom (2018). Workers’ health and productivity under occupational heat strain: A systematic review and meta-analysis. Lancet Planet. Health. 2:e521–31.
Foster, J., J. Smallcombe, S. Hodder, O. Jay, A. Flouris, L. Nybo, and G. Havenith (2021). An advanced empirical model for quantifying the impact of heat and climate change on human physical work capacity. Int. J. Biometeorol. 65:1215-1229.
Girgis, N., S. Elariane, and M.A. Elrazik (2016). Evaluation of heat exhausts impacts on pedestrian thermal comfort. Sustain. Cities Soc. 27:152–159.
Glaser, J., E. Hansson, I. Weiss, C. Wesseling, K. Jakobsson, U. Ekström, J. Apelqvist, R. Lucas, E. Arias Monge, S. Peraza, C. Hogstedt, and D.H. Wegman (2020). Preventing kidney injury among sugarcane workers: Promising evidence from enhanced workplace interventions. Occup. Environ. Med. 77:527–534.
Hew-Butler, T., V. Smith-Hale, A. Pollard-McGrandy, and M. VanSumeren (2019). Of mice and men—the physiology, psychology, and pathology of overhydration. Nutrients 11:1539.
Hospers, L., J.W. Smallcombe, N.B. Morris, A. Capon, and O. Jay (2020). Electric fans: A potential stay-at-home cooling strategy during the COVID-19 pandemic this summer? Sci. Total Environ. 747:141180.
Houser, M.C., V. Mac, D.J. Smith, R.C. Chicas, N. Xiuhtecutli, J.D. Flocks, L. Elon, M.G. Tansey, J.M. Sands, L. McCauley, and V.S. Hertzberg (2021). Inflammation-related factors identified as biomarkers of dehydration and subsequent acute kidney injury in agricultural workers. Biolog. Res. Nursing. 23:676–688.
Ioannou, L.G., K. Mantzios, L. Tsoutsoubi, E. Nintou, M. Vliora, P. Gkiata, C.N. Dallas, G. Gkikas, G. Agaliotis, K. Sfakianakis, A.K. Kapnia, D.J. Testa, T. Amorim, P.C. Dinas, T.S. Mayor, C. Gao, J. Nybo, and A.D. Flouris (2021a). Occupational heat stress: Multi-country observations and interventions. Int. J. Environ. Res. Public Health. 18:6303.
Ioannou, LG., L. Tsoutsoubi, K. Mantzios, G. Gkikas, J.F. Piil, P.C. Dinas, S.R. Notley, G.P. Kenny, L. Nybo, and A.D. Flouris (2021b). The impacts of sun exposure on worker physiology and cognition: multi-country evidence and interventions. Int. J. Environ. Res. Public Health. 18:7698.
Jay, O., M.N. Cramer, N.M. Ravanelli, and S.G. Hodder (2015). Should electric fans be used during a heat wave? Appl. Ergonom. 46::137–143.
Kaufman, C., M.C. Morrissey-Basler, M. Marcelino, and D.J. Casa (2025). The Effects of Body Cooling Strategies on
Physiological and performance outcomes during simulated occupational work in the heat. Am. J. Ind. Med.
doi: 10.1002/ajim.23734. Online ahead of print.
Kenefick, R.W., and M.N. Sawka (2007). Hydration at the work site. J. Am. Coll. Nutr. 26(5 Suppl): 597S-603S.
Krisher, L., J. Butler-Dawson, H. Yoder, D. Pilloni, M. Dally, E.C. Johnson, D. Jaramillo, A. Cruz, C. Asensio, and L.S. Newman (2020). Electrolyte beverage intake to promote hydration and maintain kidney function in Guatemalan sugarcane workers laboring in hot conditions. J. Occup. Environ. Med. 62:e696–703.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009 May 05;150(9):604–12.https://doi.org/10.7326/0003-4819- 15 0 - 9 -2 0 0 9 0 5 0 5 0 - 00006.
Lopez, R.M., D.J. Casa, K.A. Jensen, J.K. DeMartini, K.D. Pagnotta, R.C. Ruiz, M.W. Roti, R.L. Stearns, L.E. Armstrong, and C.M. Maresh (2011). Examining the influence of hydration status on physiological responses and running speed during trail running in the heat with controlled exercise intensity. J. Strength Cond. Res. 25: 2944–2954.
Mix, J., L. Elon, V.V.T. Mac, J. Flocks, E. Economos, A.J. Tovar-Aguilar, V.S. Hertzberg, and L.A. McCauley (2018). Hydration status, kidney function, and kidney injury in Florida agricultural workers. J. Occup. Environ. Med. 60:e253–e260.
Morabito, M., A. Messeri, A. Crisci, J. Bao, R. Ma, S. Orlandini, C. Huang, and T. Kjellstrom (2020). Heat-related productivity loss: benefits derived by working in the shade or work-time shifting. Int. J. Productiv. Perform. Management. 70:507–525.
Morris, N.B., T. English, L. Hospers, A. Capon, and O. Jay (2019). The effects of electric fan use under differing resting heat index conditions: A clinical trial.” Ann. Intern. Med. 171:675–677.
Morris, N.B., O. Jay, A.D. Flouris, A. Casanueva, C. Gao, J. Foster, G. Havenith, and L. Nybo (2020). Sustainable solutions to mitigate occupational heat strain – an umbrella review of physiological effects and global health perspectives. Environ. Health. 19:95.
Morrissey. M.C., D.J. Casa, G.J. Brewer, W.M. Adams, Y. Hosokawa, C.L. Benjamin, A.J. Grundstein, D. Hostler, B.P. McDermott, M.L. McQuerry, R.L. Stearns, E.M. Filep, D.W. DeGroot, J. Fulcher, A.D. Flouris, R.A. Huggins, B.L. Jacklitsch, J.F. Jardine, R.M. Lopez, R.B. McCarthy, Y. Pitisladis, R.R. Pryor, Z.J. Schlader, C.J. Smith, D.L. Smith, J.T. Spector, J.K. Vanos, W.J. Williams, N.T. Vargas, and S.W. Yeargin (2021a). Heat safety in the workplace: modified delphi consensus to establish strategies and resources to protect U.S workers. GeoHealth. 5:e2021GH000443.
Morrissey, M.C., G.J. Brewer, W.J. Williams, T. Quinn, and D.J. Casa (2021b). Impact of occupational heat stress on worker productivity and economic cost. Am. J. Indust. Med. 64:981-988.
Morrissey-Basler, M.C., C.M. Eason, S.H. Clines, C.E. Kaufman, and D.J. Casa (2023). Perceived challenges and barriers for females working in the heat. J. Occup. Environ. Hyg. 21:97-107.
Morrissey-Basler, M.C., G.J. Brewer, T. Anderson, W.M. Adams, J.S. Navarro, M. Marcelino, D.G, Martin, and D.J. Casa (2024). The effect of heat mitigation strategies on thermoregulation and productivity during simulated occupational work in the heat in physically active young men. Front. Sports Act. Living. 5:1274141.
National Institute for Occupational Safety and Health (NIOSH). (2016). Criteria for a recommended standard: Occupational exposure to heat and hot environments (NIOSH Publication No. 2016-106). U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention. http://www.cdc.gov/niosh/docs/2016-106/
Natural Resources Defense Council (NRDC) (2024). Occupational heat safety standards in the United States. https://www.nrdc.org/resources/occupational-heat-safety-standards-united-states
Nerbass, F.B., L. Moist, W.F. Clark, M.A. Vieira, and R. Pecoits-Filho (2019). Hydration status and kidney health of
factory workers exposed to heat stress: A pilot feasibility study. Ann. Nutr. Metab. 74(Suppl. 3): 30–37.
Occupational Safety and Health Administration (OSHA) (2011). Water. Rest. Shade. U.S. Department of Labor.
https://www.osha.gov/heat
Otani, H., M. Kaya, A. Tamaki, H. Goto, K. Tokizawa, and R.J. Maughan (2021). Combined effects of solar radiation and airflow on endurance exercise capacity in the heat. Physiol. Behav. 229:113264.
Otani, H., M. Kaya, A. Tamaki, Y. Hosokawa, and J.K. W. Lee. (2019). Solar radiation and the validity of infrared tympanic temperature during exercise in the heat. Int. J. Biometeorol. 64:39-45.
Piil, J.F., J. Lundbye-Jensen, L. Christiansen, L. Ioannou, L. Tsoutsoubi, C.N. Dallas, K. Mantzios, A.D. Flouris, and L. Nybo (2018). High prevalence of hypohydration in occupations with heat stress-perspectives for performance in combined cognitive and motor tasks. PloS One. 13:e0205321.
Sawka, M.N., and S.J. Montain (2000). Fluid and electrolyte supplementation for exercise heat stress1234. Am. J. Clin. Nutr. 72(Suppl):564S-572S.
Stoecklin-Marois, M., T. Hennessy-Burt, D. Mitchell, and M. Schenker (2013). Heat-related illness knowledge and practices among California hired farm workers in the MICASA study. Industr. Health. 51:47–55.
Venugopal, V., S. Rekha, K. Manikandan, P.K. Latha, V. Vennila, N. Ganesan, P. Kumaravel, and S.J. Chinnadurai (2016). Heat stress and inadequate sanitary facilities at workplaces - an occupational health concern for women? Global Health Action. 9:31945.
Wagoner, R.S., N.I. López-Gálvez, J.G. de Zapien, S.C. Griffin, R.A. Canales, and PI. Beamer (2020). An occupational heat stress and hydration assessment of agricultural workers in north Mexico. Int. J. Environ. Res. Public Health. 17:2102.
Wästerlund, D.S., J. Chaseling, and L. Burström (2004). The effect of fluid consumption on the forest workers’ performance strategy. Appl. Ergonom. 35:29–36.
Wegman, D.H., J. Apelqvist, M. Bottai, U. Ekström, R. García-Trabanino, J. Glaser, C. Hogstedt, K. Jakobsson, E. Jarquín, R.A.I. Lucas I. Weiss, C. Wesseling, T. Bodin; Work Health and Efficiency (WE) Program Working Group (2018). Intervention to diminish dehydration and kidney damage among sugarcane workers. Scand. J. Work Environ. Health. 44:16–24.
Wesseling, C., A. Aragón, M. González, I. Weiss, J. Glaser, C.J. Rivard, C. Roncal-Jiménez, R. Correa-Rotter, and R.J. Johnson (2016). Heat stress, hydration and uric acid: a cross-sectional study in workers of three occupations in a hotspot of Mesoamerican nephropathy in Nicaragua. BMJ Open. 6:e011034.
World Health Organization (WHO) (2006). Oral rehydration salts. https://www.who.int/ publications/i/item/WHO-FCH-CAH-06.1.
WHO Scientific Group on Health Factors Involved in Working under Conditions of Heat (1969). Health factors involved in working under conditions of heat stress: Report of a WHO Scientific Group. https://iris.who.int/handle/10665/40716.








