KEY POINTS
- There is a lack of extensive research on the impact of heat exposure and effectiveness of heat stress prevention strategies in working populations. Findings from sports research cannot be directly applied to the occupational setting.
- Occupational heat exposure can lead to both acute and chronic health and safety consequences, including excessive fatigue, heat syncope, heat exhaustion, exertional heat stroke, increased accidents, kidney injury, cardiac mortality and the potential for a myriad of other health outcomes.
- There is an emerging understanding of an epidemic of chronic kidney disease of nontraditional etiology and occupational origin (CKDnT), which occurs in the absence of traditional risk factors. The prevalence is particularly high among young male workers in low-income countries.
- Early detection and intervention of heat-related health conditions is critical to improve health outcomes for workers exposed to heat stress.
- Work-related productivity losses due to heat exposure represent a significant economic burden, driven by reductions in physical work capacity, increased lost work time, lost wages and higher treatment and rehabilitation costs.
INTRODUCTION
Workers are frequently termed "industrial athletes" because of the physically strenuous tasks they undertake daily (Astrand et al., 1975; Binazzi et al., 2019; Flouris et al., 2018). In contrast to most athletes (Figure 1), workers face a combination of environmental heat exposure and high physical workloads with insulating personal protective equipment (PPE) over consecutive days without the adequate rest, recovery and resources that most athletes have available (Astrand et al., 1975). This combination significantly intensifies heat strain on the body, (Flouris et al. 2018; Ioannou et al., 2021a,b) placing workers at greater risk of succumbing to heat-related injuries, illnesses and fatalities. Every year, 2.41 billion workers are exposed to excessive heat, resulting in 22.85 million occupational injuries and 18,970 deaths worldwide (International Labour Organization (ILO), 2024). Alarmingly, 90% of worker exposure to excessive heat occurs outside of a heatwave (ILO, 2024). Occupational heat strain jeopardizes worker health and safety, resulting in adverse impacts on productivity. Heat-related productivity losses impose a significant strain on the economy, impairing both worker and organizational performance and success. By 2030, global economic losses from occupational heat stress are projected to reach $2.4–2.5 trillion USD (Borg et al., 2021). As climate change progresses, the frequency, intensity and severity of heat events are expected to worsen (Gao et al., 2018), further amplifying the adverse impacts on health, safety and productivity (Morrissey et al., 2021b).
Although occupational heat exposure significantly affects workers, there is a lack of extensive research on the health and physiological impacts of working in heat, as well as effective heat mitigation strategies to reduce heat strain. Furthermore, the diversity between occupations and within worksites presents additional challenges to applying general recommendations. In the United States, much of the existing heat physiology research has been concentrated on sports and military populations (8 and 1.3 million, respectively), while ~11 million documented workers are routinely exposed to hot work environments, which is likely an underestimate (Governing, 2013; ILO, 2024). While research in sports and military settings has made notable advancements in understanding and managing heat strain, these findings cannot be directly transferred to the occupational setting. For example, workers have a high prevalence of poor health conditions such as hypertension, cardiovascular disease, diabetes and obesity, which negatively impact physiological and thermoregulatory function under heat stress (Ali & Mohammadnezhad, 2019; Bamidele et al., 2024; Hertz et al., 2004; Kenny et al., 2013; Morrissey et al., 2021c; Notley et al., 2021). In some work settings, workers cannot miss work or change their schedule of work due to high heat conditions because of financial concerns. Also, in remote settings, there is limited access to medical care if a heat emergency were to occur. Therefore, it is critically important to expand our understanding on how occupational heat exposure acutely and chronically impacts worker health, safety and productivity.
This Sport Science Exchange (SSE) article will outline our current understanding of the acute and long-term issues associated with working in the heat. This article will serve as a “Part 1” of a two-part article series and “Part 2” will explore heat stress mitigation strategies to reduce occupational heat strain.

ACUTE AND LONG-TERM HEALTH AND SAFETY EFFECTS
Workers often engage in physically demanding work in hot environments and are often required to wear PPE to avoid other workplace hazards (Bernard & Ashley 2009; Gao et al., 2018). This can result in many adverse health and safety outcomes (Crowe et al., 2023). When humans undergo physical work in the heat, the body maintains its temperature through thermoregulatory mechanisms, which includes skin vasodilation and eccrine sweating (Périard et al., 2021). It is the body’s natural response to experience a rise in core temperature while engaging in physical work, however, when the metabolic heat generated by the body outweighs its ability to dissipate heat, this can result in continuous and a potentially dangerous rise in core temperature (Foster et al., 2020). High core temperatures have serious implications for the health and safety of workers exposed to heat, which range from discomfort, heat syncope, heat exhaustion, to life-threatening medical conditions such as exertional heat stroke (EHS) (Figure 2) (Casa et al., 2015). EHS is considered a medical emergency and is characterized as a core temperature over >40ºC and presents with central nervous system dysfunction (Casa et al., 2015). While reported occupational EHS cases are low, if left untreated, EHS can result in permanent complications or even death (US Department of Labor, 2020). For example, the Bureau of Labor Statistics reported an average of 34 deaths/year between 1992-2022 (Bureau of Labor Statistics, 2025). However, it's important to recognize that these cases are only reported instances and may not reflect the actual number of heat-related illnesses in the workplace. EHS and other heat-related illnesses might not always be correctly categorized or identified as such, and unfortunately, many employers may fail to report EHS-related fatalities, especially among undocumented workers (Morrissey et al., 2023). Moreover, occupational health and safety agencies may only require the proximal cause of death to be reported. This limits our understanding of the full impact of heat in the workplace, as heat can lead to cognitive impairments and neuromuscular dysfunction, both of which contribute to an increased risk of accidents (Mazlomi et al., 2017; Thompson et al., 2023).
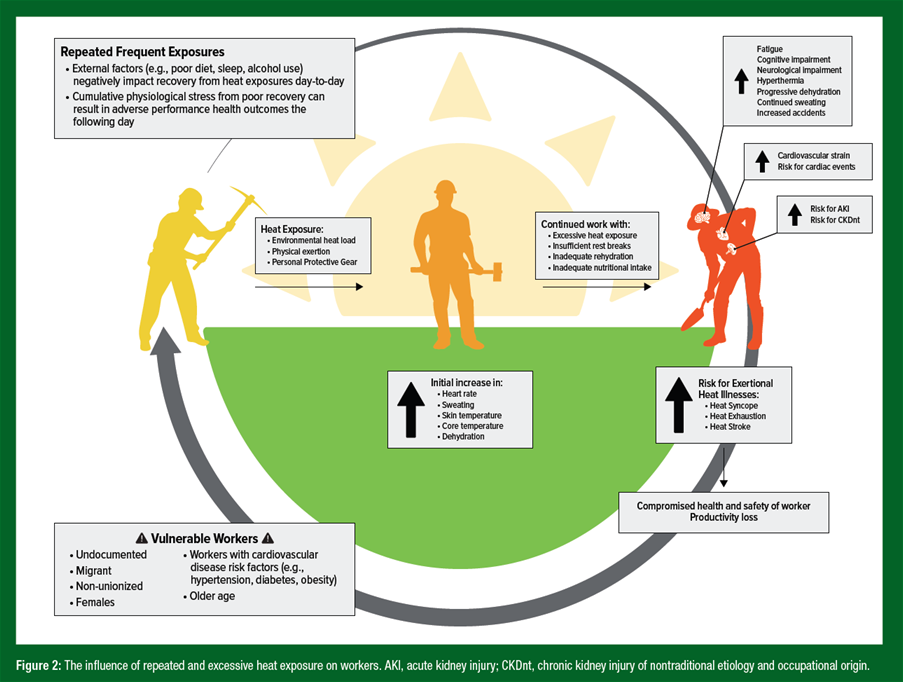
Working in the heat also has a profound effect on worker physiology, increasing skin temperature, heart rate, sweating and fatigue (Crowe et al., 2023; Périard et al., 2021). Increased sweating without adequate fluid replacement can further exacerbate a rise in heart rate (Cheuvront & Kenefick, 2014; Kenefick & Sawka, 2007; Adams et al., 2014), core temperature (Cheuvront & Kenefick, 2014; Cheuvront et al., 2010) and risk of acute kidney injury (AKI) (Chapman et al., 2020). AKI is characterized as a rapid reduction in kidney function and can be induced by increases in core temperature (>38.5°C; hyperthermia) and dehydration without adequate fluid replacement (Chapman et al., 2020; Junglee et al., 2013; Schlader et al., 2017). Markers of AKI risk increase following physical work in the heat and are augmented as core temperatures rise and dehydration progresses (Chapman et al., 2020). Currently, there is an epidemic of chronic kidney disease (CKD) among laborers who perform heavy physical work in hot environments (Johnson et al., 2019). In 2020, 26.2 million workers were living with heat-related chronic kidney disease, classified as CKD of nontraditional etiology and occupational origin (CKDnt) (ILO, 2024). CKDnt is prevalent among laborers in agriculture, construction and mining, and tends to occur in the absence of traditional CKD risk factors such as age, hypertension, obesity or diabetes (Chapman et al., 2019; Gallo- Ruiz et al., 2019; Wesseling et al., 2020). Many individuals with CKDnt do not exhibit early clinical symptoms, which makes early detection and screening very difficult (Amorim & Schlader 2025; Chapman et al., 2019; Whaley-Connell et al., 2011). Elevated core temperature, dehydration, and exposure to environmental factors such as metals and pesticides, can lead to a reduction in renal blood flow, resulting in renal ischemia, inflammation and oxidative stress (Chapman et al., 2019; Gallo-Ruiz et al., 2019; Masoud et al., 2024; Venugopal et al., 2024). The kidneys are often required to increase their metabolic demand to regulate water and electrolyte balance which further exacerbates these effects (Chapman et al., 2021) (Figure 3). Unfortunately, clinical symptoms often become present when the disease has progressed, and substantial kidney damage has already occurred. There is a particularly high number of young male laborers in low-income countries who experience CKDnt (Stanifer et al., 2016). Young laborers in low-income countries or those who migrate for work are also reported to have high risk of cardiac mortality during periods of high heat exposure (Pradhan et al., 2019). In conclusion, it is clear that occupational heat exposure can lead to substantial negative health outcomes in workers, both short and long term.

PRODUCTIVITY AND PERFORMANCE EFFECTS
Labor productivity and economic success are significantly impacted by occupational heat stress (Messieh, 2021; Borg et al., 2021; Park et al., 2017; Orlov et al., 2019). It is predicted that the global cost of lost worktime associated with occupational heat exposure will rise to $2.4-2.5 trillion in 2030 (>1% of gross domestic product (GDP)) from 311 billion in 2010 (~0.5% of GDP), which is a 557% increase (Borg et al., 2021). A meta-analysis in 11 studies of a total of 8076 workers estimated a 30% prevalence of productivity losses due to occupational heat stress (Flouris et al., 2018). Seven of the included studies reported a 2.6% decrease for every degree increase in wet bulb globe temperature above 24°C (Flouris et al., 2018). In the United States, occupational heat exposure could result in a loss of $100 billion annually (Messieh, 2021). Without implementing effective occupational heat stress mitigation interventions, heat-related labor productivity losses could double to $200 billion by 2030 and reach $500 billion by 2050 (Messieh, 2021).
There are several factors that cause labor productivity losses induced by occupational heat stress. Machinery mechanical failures, infrastructure system failures and agricultural yield loss are mechanisms associated with labor productivity losses, however, these factors are not directly linked to worker health, safety and work capacity (Messieh, 2021). Worker-related labor productivity losses associated with heat stress include both presenteeism and absenteeism (Morrissey et al., 2021b) (Figure 4). Heat-related presenteeism can be defined as losses in productivity when workers are not fully functioning in their workplace, and therefore, have reductions in their physical work capacity (Morrissey, Brewer, et al. 2021). Reductions in physical work capacity can be induced by factors such as impaired cognitive performance, dehydration, hyperthermia, increased discomfort and fatigue (Morrissey et al., 2021b). Occupational heat exposure can also impact the work environment. For example, safety goggles can fog, sweat can get in workers’ eyes and sweaty hands can reduce grip on tools, leading to increased risk of accidents (Morrissey et al., 2021b). Ultimately, physiological, cognitive, perceptual and physical changes in the environment induced by occupational heat exposure can reduce the overall work output, the quality of work and increase time off task.

Heat stress can also impact productivity through heat-related absenteeism (Morrissey et al., 2021b). Heat-related absenteeism is characterized as a worker’s absence from work due to the adverse effects of heat. Absenteeism associated with heat exposure can occur due to heat-related illnesses, workplace injuries and fatalities. When illnesses and injuries occur, employers are subjected to worker compensation claims insurance payouts, medical fees (i.e., healthcare costs related to treatment and rehabilitation), subsidies and additional expenses to hire and train new staff members (Borg et al., 2021; Martínez-Solanas et al., 2018; Morrissey et al., 2021b). Employers also face the risk of lawsuits related to long-term health issues and fatalities caused by heat exposure. Interventions to mitigate occupational heat exposure are typically low-cost, and heat-related deaths can be prevented through evidence-based heat stress management strategies and emergency procedures (Casa et al., 2015; Demartini et al., 2015). Workers are also susceptible to financial burdens as heat-related illnesses and injuries can result in lost salaries and wages. Borg et al. (2021) reported there was a greater cost for workers in low and middle-income countries, outdoor industries, medium-sized businesses and workers between 25-45 years old. In response to these productivity and economic concerns, effective and practical heat mitigation solutions are urgently needed to safeguard workers health and safety and limit threats to productivity (Morris et al., 2020; Morrissey et al., 2021a).
PRACTICAL APPLICATIONS
- Understanding the health, safety and productivity impacts of occupational heat stress is the foundational step to creating the solutions to implement to protect workers. As such, the following practical applications are proposed and will be expanded upon in “Part 2”:
- Do not directly apply heat physiology research from sport to the occupational setting (Figure 1).
- Understanding the substantial occupational health and safety effects of heat stress on workers is crucial to improve short-term and long-term health and safety outcomes and enhance productivity and economic success (Figure 2).
- Methods of early detection and intervention of health conditions, such as CKDnt, should be considered to better protect vulnerable workers.
SUMMARY
It is essential to enhance our understanding of the acute and chronic effects of occupational heat exposure on worker health, safety and productivity. While research in sports settings has advanced knowledge about the impact of heat, the differences between athletes and working populations demonstrate that these findings should not be directly applied to occupational environments. Occupational heat exposure can cause immediate health and safety issues, such as discomfort, fatigue, heat syncope and an increased risk of accidents. Excessive heat exposure can lead to exertional heat stroke, a life-threatening condition that requires immediate treatment to prevent permanent damage or death. Additionally, there are significant long-term health consequences, such as acute kidney injury resulting from hyperthermia and dehydration, which can lead to chronic kidney disease (CKD). In workers, particularly young males in low-income countries, there is a rising epidemic of chronic kidney disease of non-traditional causes (CKDnt), often occurring in the absence of typical risk factors and without symptoms until the disease has advanced. Early detection and intervention for CKDnt and other heat-related conditions are critical. Moreover, occupational heat exposure negatively impacts productivity by reducing physical work capacity, increasing lost work time and leading to lost wages and higher healthcare costs for treatment and rehabilitation, resulting in a substantial economic burden. In response to health, safety and productivity decrements, effective heat stress mitigation strategies must be developed and implemented to adequately protect workers.
The views expressed are those of the authors and do not necessarily reflect the position or policy of PepsiCo, Inc.
REFERENCES
Adams, W.M., E.M. Ferraro, R.A. Huggins, and D.J. Casa (2014). Influence of body mass loss on changes in heart rate during exercise in the heat: A systematic review. J. Strength Cond. Res. 28:2380–2389.
Ali, R.M., and M. Mohammadnezhad (2019). prevalence of metabolic syndrome among apparently healthy workforce. J. Ayub Med. Coll. 31:252–264.
Amorim, F., and Z. Schlader (2025). The kidney under heat stress: A vulnerable state. Curr. Opin. Nephrol. Hyperten. 34:170–176.
Astrand, I., O. Axelson, U. Eriksson, and L. Olander (1975). Heat stress in occupational work. Ambio. 4:37–42.
Bamidele, A.A., N.L. Ferreira, A. Gupta, and Z. Khan (2024). Prevalence and mitigation of cardiovascular disease risk factors among the corporate workforce in sub-Saharan Africa: A systematic review and meta-Analysis. Cureus 16:e75888.
Bernard, T.E., and C.D. Ashley (2009). Short-term heat stress exposure limits based on wet bulb globe temperature adjusted for clothing and metabolic rate. J. Occup. Environ. Hygiene. 6:632–638.
Binazzi, A., M. Levi, M. Bonafede, M. Bugani, A. Messeri, M. Morabito, A. Marinaccio, and A. Baldasseroni (2019). Evaluation of the impact of heat stress on the occurrence of occupational injuries: Meta-analysis of observational studies. Am. J. Indust. Med. 62:233–243.
Borg, M.A., J. Xiang, O. Anikeeva, D. Pisaniello, A. Hansen, K. Zander, K. Dear, M.R. Sim, and P. Bi (2021). Occupational heat stress and economic burden: A review of global evidence. Environ. Res. 195:110781.
Bureau of Labor Statistics (2025). IIF Home. Accessed March 10, 2025. https://www.bls. gov/iif/.
Casa, D.J., J.K. DeMartini, M.F. Bergeron, D. Csillan, E.R. Eichner, R.M. Lopez, M.S. Ferrara, K.C. Miller, F. O'Connor, M.N. Sawka, and S.W. Yeargin (2015). National Athletic Trainers’ Association position statement: Exertional heat illnesses. J. Athl. Train. 50:986–1000.
Chapman, C.L., B.D. Johnson, N.T. Vargas, D. Hostler, M.D. Parker, and Z.J. Schlader (2020). Both hyperthermia and dehydration during physical work in the heat contribute to the risk of acute kidney injury. J. Appl. Physiol. 128: 715–728.
Chapman, C.L., B.D. Johnson, M.D. Parker, D. Hostler, R.R. Pryor, and Z. Schlader. (2021). Kidney physiology and pathophysiology during heat stress and the modification by exercise, dehydration, heat acclimation and aging. Temperature. 8:108–159.
Chapman, E., M.M. Haby, E. Illanes, J. Sanchez-Viamonte, V. Elias, and L. Reveiz (2019). Risk factors for chronic kidney disease of non-traditional causes: A systematic review. Rev. Panam. de Salud Públ. 43:e35.
Cheuvront, S.N., R.W. Kenefick, S.J. Montain, and M. N. Sawka (2010). Mechanisms of aerobic performance impairment with heat stress and dehydration. J. Appl. Physiol. 109:1989–1995.
Cheuvront, S.N., and R.W. Kenefick (2014). Dehydration: Physiology, assessment, and performance effects. Compr. Physiol. 4:257–285.
Crowe, J., B. Knechtle, and D. Rojas-Valverde (2023). Editorial: Acute and long-term health issues of occupational exposure to heat and high physical loads. Front. Physiol. 14:1304229.
Demartini, J.K., D.J. Casa, R. Stearns, L. Belval, A. Crago, R.B. Davis, and J. Jardine (2015). Effectiveness of cold water immersion in the treatment of exertional heat stroke at the Falmouth road race. Med. Sci. Sports Exerc. 47:240–245.
Flouris, A.D, P.C. Dinas, L.G. Ioannou, L. Nybo, G. Havenith, G.P. Kenny, and T. Kjellstrom (2018a). Workers’ health and productivity under occupational heat strain: A systematic review and meta-analysis. Lancet Planetary Health. 2:e521–531.
Foster, J., S.G. Hodder, A.B. Lloyd, and G. Havenith (2020). Individual responses to heat stress: Implications for hyperthermia and physical work capacity. Front. Physiol. 11:541483.
Gallo-Ruiz, L., C. M. Sennett, M. Sánchez-Delgado, A. García-Urbina, T. Gámez-Altamirano, K. Basra, R.L. Laws, J.J. Amador, D. Lopez-Pilarte, Y. Tripodis, D.R. Brooks, M.D. McClean, J. Kupferman, D. Friedman, A. Aragón, M. González-Quiroz, and M.K. Scammell (2019). Prevalence and risk factors for CKD among brickmaking workers in La Paz Centro, Nicaragua. Am. J. Kidn. Dis. 74:239–247.
Gao, C., K. Kuklane, P.O. Östergren, and T. Kjellstrom (2018). Occupational heat stress assessment and protective strategies in the context of climate change. Int. J. Biometeorol. 62:359–371.
Governing (2013). Military active-duty personnel, civilians by state. 2013. October 3, 2013. https://www.governing.com/archive/military-civilian-active-duty-employee-workforce-numbers-by-state.html.
Hertz, R.P., A.N. Unger, M. McDonald, M.B. Lustik, and J. Biddulph-Krentar (2004). The impact of obesity on work limitations and cardiovascular risk factors in the U.S. workforce. J. Occup. Environ. Med. 46:1196.
International Labour Organization (ILO) (2024). Heat at work; Implications for safety and health: A global review of the science, policy and practice. Geneva.
Ioannou, L,G., K. Mantzios, L. Tsoutsoubi, E. Nintou, M. Vliora, P. Gkiata, C.N. Dallas, G. Gkikas, G. Agaliotis, K. Sfakianakis, A.K. Kapnia, D.J. Testa, T. Amorim, P.C. Dinas, T.S. Mayor, C. Gao, L. Nybo, and A.D. Flouris (2021a). Occupational heat stress: Multi-country observations and interventions. Int. J. Environ. Res. Public Health. 18:6303.
Ioannou, L.G., L. Tsoutsoubi, K. Mantzios, G. Gkikas, J.F. Piil, P.C. Dinas, S.R. Notley, G.P. Kenny, L. Nybo, and A.D. Flouris (2021b). The impacts of sun exposure on worker physiology and cognition: Multi-country evidence and interventions. Int. J. Environ. Res. Public Health. 18:7698.
Johnson, R.J., C. Wesseling, and L.S. Newman (2019). Chronic kidney disease of unknown cause in agricultural communities. New Eng. J. Med. 380:1843–1852.
Junglee, N.A., U. Di Felice, A. Dolci, M.B. Fortes, M.M. Jibani, A.B. Lemmey, N.P. Walsh, and J.H. Macdonald (2013). Exercising in a hot environment with muscle damage: Effects on acute kidney injury biomarkers and kidney function. Am. J. Physiol. 305: F813– F820.
Kenefick, R.W., and M.N. Sawka (2007). Hydration at the work site. J. Am. Coll. Nutr. 26(5 Suppl): 597S-603S.
Kenny, G.P., J.M. Stapleton, J.E. Yardley, P. Boulay, and R.J. Sigal (2013). Older adults with type 2 diabetes store more heat during exercise. Med. Sci. Sports Exerc. 45:1906– 1914.
Martínez-Solanas È., M. López-Ruiz, G.A. Wellenius, A. Gasparrini, J. Sunyer, F.G. Benavides and X. Basagaña (2018). Evaluation of the impact of ambient temperatures on occupational injuries in Spain. Env. Health Persp. 126:067002.
Masoud, A., Z.J. McKenna, Z. Li, M.R. Deyhle, C.M. Mermier, Z.J. Schlader, and F. T. Amorim (2024). Strategies to mitigate acute kidney injury risk during physical work in the heat. Am. J. Physiol. 326:F499–F510.
Mazlomi, A., F. Golbabaei, S.F. Dehghan, M. Abbasinia, S.M. Khani, M. Ansari, and M. Hosseini (2017). The influence of occupational heat exposure on cognitive performance and blood level of stress hormones: A field study report. Int. J. Occup. Safety Ergonom. 23:431–439.
Messieh, N. (2021). Extreme heat: The economic and social consequences for the United States.” Atlantic Council (blog). August 31, 2021. https://www.atlanticcouncil.org/in-depth-research-repor ts/repor t /ex treme-heat-the-economic-and-social-consequences-for-the-united-states/.
Morris, N.B., O. Jay, A.D. Flouris, A. Casanueva, C. Gao, J. Foster, G. Havenith, and L. Nybo (2020). Sustainable solutions to mitigate occupational heat strain – An umbrella review of physiological effects and global health perspectives. Environ. Health. 19:95.
Morrissey, M.C., D.C. Casa, G.J. Brewer, W.M. Adams, Y. Hosokawa, C.L. Benjamin, A.J. Grundstein, D. Hostler, B.P. McDermott, M.L. McQuerry, R.L. Stearns, E.M. Filep, D.W. DeGroot, J. Fulcher, A.D. Flouris, R.A. Huggins, B.L. Jacklitsch, J.F. Jardine, R.M. Lopez, R.B. McCarthy, Y. Pitisladis, R.R. Pryor, Z.J. Schlader, C.J. Smith, D.L. Smith, J.T. Spector, J.K. Vanos, W.J. Williams, N.T. Vargas, and S.W. Yeargin (2021a). Heat safety in the workplace: Modified delphi consensus to establish strategies and resources to protect U.S workers. Geohealth. 5:e2021GH000443.
Morrissey, M.C., G.J. Brewer, W.J. Williams, T. Quinn, and D.J. Casa (2021b). Impact of occupational heat stress on worker productivity and economic cost. Am. J. Ind. Med. 64:981-988.
Morrissey, M.C., Y. Wu, E.F. Zuk, J. Livingston, D.J. Casa, and L.S. Pescatello (2021c). The impact of body fat on thermoregulation during exercise in the heat: A systematic review and meta-analysis. J. Sci. Med. Sport. 24:843–850.
Morrissey, M.C., Z.Y. Kerr, G.J. Brewer, F. Tishukaj, D.J. Casa, and R.L. Stearns (2023). Analysis of exertion-related injuries and fatalities in laborers in the United States. Int. J. Environ. Res. Public Health. 20:2683.
Notley, S.R., A.P. Akerman, B.J. Friesen, M.P. Poirier, R.J. Sigal, A.D. Flouris, P. Boulay, E. McCourt, M. Ruzicka, and G.P. Kenny (2021). Heat tolerance and occupational heat exposure limits in older men with and without type 2 diabetes or hypertension. Med. Sci. Sports Exerc. 53:2196–2206.
Orlov, A., J. Sillmann, A. Aaheim, K. Aunan, and K. de Bruin (2019). Economic losses of heat-induced reductions in outdoor worker productivity: A case study of Europe. Econ. Disast. Climate Change. 3:191–211.
Park, J., Y. Kim, and I. Oh (2017). Factors affecting heat-related diseases in outdoor workers exposed to extreme heat. Annals Occup. Environ. Med. 29:30.
Périard, J.D., T.M.H. Eijsvogels, and H.A.M. Daanen (2021). Exercise under heat stress: Thermoregulation, hydration, performance implications, and mitigation strategies. Physiol. Rev. 101:1873–1979.
Pradhan, B., T. Kjellstrom, D. Atar, P. Sharma, B. Kayastha, G. Bhandari, and P.K. Pradhan (2019). Heat stress impacts on cardiac mortality in Nepali migrant workers in Qatar. Cardiology. 143:37–48.
Schlader, Z.J., D. Colburn, and D. Hostler (2017). Heat strain is exacerbated on the second of consecutive days of fire suppression. Med. Sci. Sports Exerc. 49:999–1005.
Stanifer, J.W., A. Muiru, T.H. Jafar, and U.D. Patel (2016). Chronic kidney disease in low- and middle-income countries. Nephr. Dial. Transplant. 31:868–874.
Thompson, C., L. Ferrie, S.J. Pearson, B. Highlands, and M.J. Matthews (2023). Do extreme temperatures affect cognition? A short review of the impact of acute heat stress on cognitive performance of firefighters. Front. Psychol. 14:1270898.
US Department of Labor (2020). “Data and Statistics | U.S. Department of Labor.” Accessed November 10, 2020. https://www.dol.gov/agencies/wb/data.
Venugopal, V., N. Damavarapu, R. Shanmugam, and P.K. Latha (2024). Occupational heat exposure and its impact on kidney health among cashew workers. J. Nephrol. 37:2007–2016.
Wesseling, C., J. Glaser, J. Rodríguez-Guzmán, I. Weiss, R. Lucas, S. Peraza, A. S. da Silva, E. Hansson, R.J. Johnson, C. Hogstedt, D.H. Wegman, and K. Jakobsson 2020. Chronic kidney disease of non-traditional origin in mesoamerica: a disease primarily driven by occupational heat stress. Rev. Panam. de Salud Públ. 44:e15.
Whaley-Connell, A., R. Nistala, and K. Chaudhary (2011). The importance of early identification of chronic kidney disease. Miss. Med. 108:25–28.