KEY POINTS
-
Dehydration on a magnitude of >2% body mass has been shown in the scientific literature to cause performance deficits. Performance deficits include areas such as aerobic and anaerobic capacity, strength, power and cognitive function, which are all crucial components in American football.
-
Planned, individualized hydration plans minimize fluid losses and help maintain a state of euhydration (normal level of hydration). These hydration plans can be easily incorporated into American football practices and competitions to maximize performance and enhance overall safety.
-
Consideration must be taken regarding the protective equipment worn by American football players and the potential extreme environmental conditions that they may be exposed to; these factors should be accounted for when developing appropriate hydration strategies for American football athletes.
-
During intense exercise in the heat, the risk of dehydration and subsequent negative influences on performance and safety risks are increased due to the exacerbation of thermoregulatory and cardiovascular strain from the excessive losses in body water.
INTRODUCTION
American football is a team sport that is characterized by short duration, high-intensity bouts of exercise followed by brief recovery periods (25-40 s) (Craig, 1968). The physical demographics of the athletes are quite variable depending on the position played; skill players are typically lean and quick, whereas the linemen are larger individuals with both larger muscle and fat masses. Depending on the league and level, all athletes must wear protective equipment during participation that is comprised of a helmet, shoulder pads and pants with hip, thigh, knee and tailbone pads. During competition, the game is split into four quarters of roughly 12-15 min each. After the second quarter there is a halftime that is between 12-20 min where athletes are permitted a break from exercise. The distance covered by football athletes is highly variable with wide receivers and defensive backs covering the most distance and linemen covering the least distance during the game. However, a tradeoff exists, in that the linemen, although they do not cover much distance during competition, are required to utilize short, high-intensity bursts of muscle power and strength (DeMartini et al., 2011). Evidence also exists to suggest that fluid needs and sweat losses are highly variable in football players (Godek et al., 2008). Linemen have been observed to lose large amounts of sweat due to their size and body mass, requiring large amounts of fluid to offset the sweat losses (Godek et al., 2008).
During exercise, the risk of dehydration is high due to increased sweat rates to aid in thermoregulation. In American football, the risk of dehydration is further increased due to the timing of the season (late summer into fall) where athletes are exposed to extreme environmental conditions (high ambient temperature and relative humidity) and the required protective equipment that may hinder heat dissipation during exercise (Armstrong et al., 2010; McCullough & Kenney, 2003). Other considerations are the size of the athletes, particularly the body surface area and overall mass of the athletes since larger individuals have a greater number of sweat glands and produce more sweat than a smaller individual (Godek et al., 2005a). It has been observed that linemen have decreased evaporative heat losses compared to non-linemen due to the relative static nature of their position and lack of airflow to the skin (Deren et al., 2014).
The combination of high environmental conditions, the requirement to wear protective equipment, and large muscle and/or fat mass increase a player’s sweat rate in order to attempt to dissipate the heat that is produced from the working muscles. During exercise, 75-80% of the energy that the working muscles use is converted to heat that is stored in the body (Shirreffs, 2005). In order to prevent body temperature from reaching dangerous levels (>40°C/104°F) that could potentially lead to exertional heat stroke (EHS), the body uses conduction, convection and evaporation of sweat from the skin to dissipate the metabolically produced heat. In high environmental conditions, evaporation of sweat from the skin is the only mode of heat dissipation from the body during exercise. The reduction in evaporative heat loss in individuals wearing American football equipment poses health and safety risks to the athletes by retaining the metabolic heat and increasing the risk of EHS. This has been evident at the high school and collegiate levels where deaths from EHS have been attributed to factors such as extreme environmental conditions and dehydration (Boden et al., 2013; Grundstein et al., 2012).
The goals of this Sports Science Exchange are to: 1) provide scientific guidelines needed to maintain a state of euhydration, 2) discuss the importance of hydration for both performance and safety in American football players and 3) provide practical recommendations for American football players, coaches and medical personnel to maintain a normal and safe hydration status during both practice and competition.
EFFECTS OF DEHYDRATION ON PHYSIOLOGICAL FUNCTION AND EXERCISE PERFORMANCE
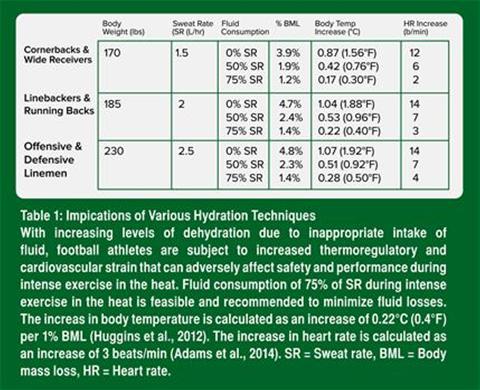
Dehydration causes both cardiovascular and thermoregulatory strain that can reduce exercise performance. During prolonged exercise, the body undergoes a physiological change called cardiovascular drift, where heart rate (HR) increases to counterbalance a decrease in stroke volume (SV) to maintain cardiac output (CO) for continued exercise. The decrease in plasma volume resulting from dehydration causes an increased HR in order to maintain the delivery of oxygen and other substrates necessary for the body’s contracting muscles (Montain & Coyle, 1992), thus exacerbating cardiovascular drift. Evidence also shows that for every 1% of body mass loss, HR increases by 3 beats/min (Adams et al., 2014).
Body temperature rises during exercise, and the rise is more pronounced with increasing levels of dehydration (Buono & Wall, 2000). Evidence has shown that for every 1% loss in body mass due to sweat losses, body temperature increases at a rate of 0.22°C (0.4°F) (Huggins et al., 2012). The increase in body temperature with increasing levels of dehydration increases thermoregulatory strain on the body, increasing the risk of exertional heat illness (Casa et al., 2012) and reducing the ability to optimally perform (Marino, 2004; Marino et al., 2004). Furthermore, increasing levels of dehydration decreases an individual’s plasma volume and sweat rate, which reduces the body’s ability to effectively dissipate heat via evaporation of sweat during exercise in the heat (Montain et al., 1998; Sawka et al., 1985).
Exercise performance is adversely affected by increasing levels of dehydration. During exercise in the heat, there are increasing demands of blood flow to both the muscles and skin to maintain muscle function and for thermoregulation. Blood flow to the skin is imperative for the body to move the metabolically produced heat to the periphery and to enable heat loss via sweating. As the level of dehydration increases, the competition over blood flow between the working muscles and skin blood flow is increased, causing a reduction in performance due to the reduction in venous pressure and cardiac output to support both the metabolic needs of exercising muscles and thermoregulation (Cheuvront & Kenefick, 2014; Cheuvront et al., 2010).
Evidence shows that dehydration impairs endurance exercise performance (Casa et al., 2010), and impairs anaerobic/high intensity performance, muscle strength, muscle power (Judelson et al., 2007a, 2007b) and cognition (Grandjean & Grandjean, 2007). These impairments are directly related to an individual’s ability to optimally perform on the athletic field, especially in American football.
HYDRATION PRACTICES AMONG AMERICAN FOOTBALL PLAYERS
Prior research has examined the hydration practices of American football players at the high school, collegiate and professional level. Overall, research has indicated that most football players, at all levels, are in a state of persistent fluid deficit (Godek et al., 2005a, 2005b, 2008; Stover et al., 2006; Yeargin et al., 2010). Godek et al. (2008) discovered that in collegiate and professional football players, average sweat rates among players ranged from 1.6-2.3 L/hr, with linemen producing greater sweat rates than the backs. When the hydration status of these athletes were monitored for multiple days, the football players were unable to replace the necessary fluids (both during practice and recovery) to return to their normal baseline hydration levels. These findings agree with other literature that has investigated the hydration status of American football players in varying levels (Godek et al., 2005a, 2005b; Stover et al., 2006).
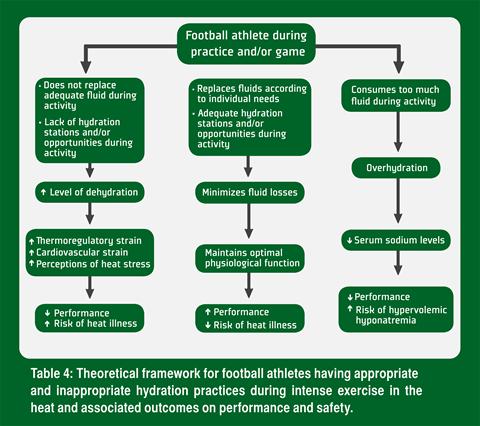
The inability to restore all fluid losses during exercise could be explained by the high fluid losses experienced by the players during practice, the inability to replace these large fluid losses during and between practices and poor hydration practices outside of practice (Stover et al., 2006). It has been observed in professional football players (unpublished data) that their hydration strategies during practice or training were adequate to replace their sweat losses, but their hydration practices outside of the training facility were poor. This resulted in football players continuously arriving to practice and training in a hypohydrated (fluid deficit) state. This caused a persistent state of hypohydration on a day-to-day basis, which can have adverse effects on performance over time. Also, during intense exercise in the heat, the implications of inappropriate hydration practices during activity can place increased thermoregulatory and cardiovascular strain on football players that can increase the risk of heat illness and cause a subsequent decline in performance (Table 1).
GUIDELINES TO MAINTAIN HYDRATION IN AMERICAN FOOTBALL
Fluid Needs During American Football
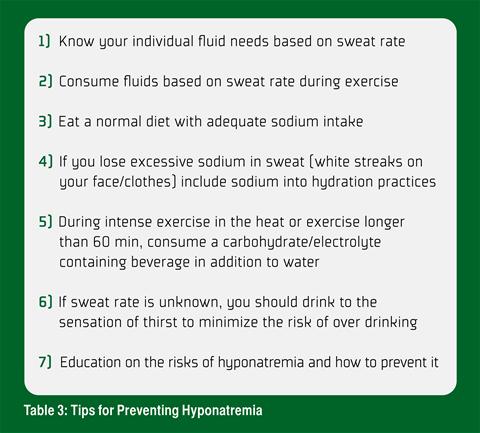
Fluid needs, especially in American football, can be highly variable per individual as mentioned earlier, making it difficult to establish general guidelines to meet the needs of all athletes (Sawka et al., 2007). The caution with general guidelines is that for some athletes who have a low sweat rate, the risk of exertional hyponatremia is large (Almond et al., 2005), whereas in athletes with large sweat rates, following general guidelines may not allow for restoration of fluid losses during exercise (Sawka et al., 2007). Others have suggested that instead of following specific guidelines that are volume dependent, athletes can drink according to the sensation of thirst to maintain a state of euhydration (Noakes, 2007). The difficulty with this strategy is that the perception of thirst typically does not appear until a level of hypohydration of ~2% body mass loss is present; a level in which performance deficits can occur-thus an individualized hydration plan may be optimal in situations in which access to fluid is not continuous. Establishing individual fluid needs based on an athlete’s sweat rate and sweat composition is recommended to minimize fluid losses and ultimately enhance performance.
Furthermore, it must be acknowledged that most athletes, especially those with high sweat rates that are commonly seen in American football players, are unable to replace all fluid losses during exercise due to the limitations of gastric emptying of the stomach. Dugas et al. (2009) reported that athletes drinking ad libitum replaced 67% of fluid losses and this did not affect performance when compared to the trials in which participants replaced 100% of fluid losses. The goal of fluid replacement during exercise is to prevent large body fluid losses that can adversely affect performance (Casa et al., 2000). The post exercise recovery period should be used to fully restore all remaining fluid losses from the exercising session (Casa et al., 2000).
Calculating Athletes Sweat Rate
Knowing one’s sweat rate is necessary to establish individual fluid needs. This can be done by having athletes weigh themselves before and after practice to determine the amount of body mass that was lost due to sweating during practice/training. More specifically, athletes should weigh themselves prior to the start of practice. During practice, athletes should have individual bottles to drink from and the total amount of fluid consumed needs to be recorded. Also, if an athlete needs to urinate during practice, the volume of urine needs to be measured. After practice, the athletes should provide a second body weight to find the difference between pre and post practice body weights. The athlete’s sweat rate can be calculated using the following equation:
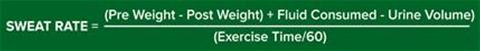
Calculating an athlete’s sweat rate should be done multiple times throughout the season to get an accurate sweat rate for every athlete; sweat rates will change depending on environmental conditions as well as whether or not the athlete is participating in a practice or game.
Hydration Strategies
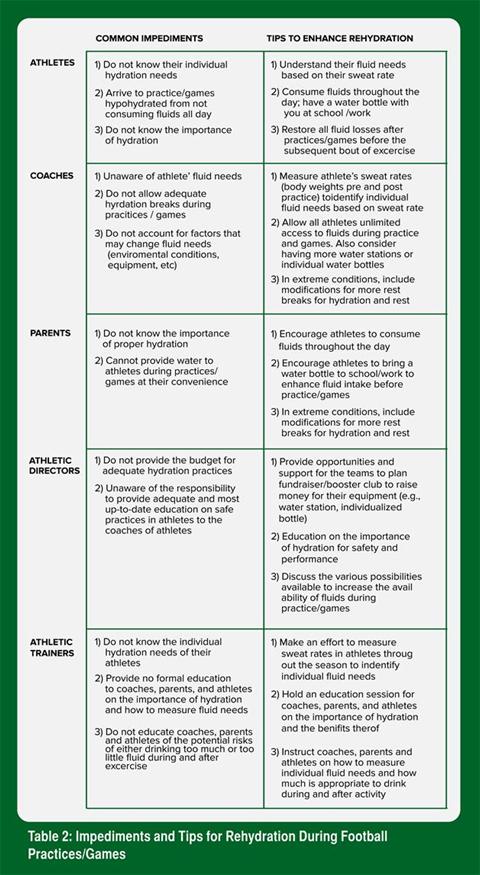
In American Football Encouraging athletes to minimize their fluid losses by drinking fluids ad libitum during exercise and replacing the remainder of the fluid losses after activity maximizes their potential for optimal performance. It is also important for the coaches and medical personnel to make modifications to practices that allow for more rest breaks for hydration according to the amount of protective equipment worn and the environmental conditions of the practice. Table 2 lists common impediments to proper hydration with associated tips to overcome these issues.
SPORTS DRINKS
Sports drinks, or drinks containing carbohydrates (CHO) and electrolytes, can be used in addition to water for rehydration purposes, especially during intense exercise in the heat lasting longer than 60 min (Casa et al., 2000). The benefit of using sports drinks in addition to water is to help restore glycogen and electrolyte levels that are lost during exercise. In addition, sports drinks with up to ~6% CHO do not slow the rate of gastric emptying which maintains the absorption of water into the body. The addition of CHO and electrolytes and unimpeded gastric emptying can help promote improved performance in athletes, especially during intense exercise (Casa et al., 2000).
HYPONATREMIA
Exertional hyponatremia is caused by the reduction of serum sodium levels in the blood (<135 mEq/L), resulting from overhydration, inadequate sodium intake or excessive sweat losses (Rosner, 2009). The reduction of serum sodium levels in blood causing exertional hyponatremia can result from overhydration, inadequate sodium intake or excessive sweat losses (Rosner, 2009). This medical condition, like EHS, can be fatal if preventive steps and appropriate treatment are not used in the event of occurrence. Although this is typically seen during long endurance events such as marathons (Almond et al., 2005; Rosner, 2009), the recent deaths of high school American football players from Georgia and Mississippi in August 2014 from exertional hyponatremia warrants further attention (Payne, 2014). Intense exercise in the heat can alter the physiological responses (increased sweat rates and altered drinking behavior) that can also increase the risk of exertional hyponatremia (Carter, 2008). Establishing individual fluid needs in addition to providing proper education for athletes, coaches, parents and medical personnel on fluid needs during physical activity is imperative to reduce the risk of hyponatremia. Furthermore, other preventive strategies can also be implemented to minimize the risk of exertional hyponatremia (Table 3).
PRACTICAL STRATEGIES
-
Educate players and coaches on the importance of maintaining euhydration to maximize performance and enhance safety during participation in American football.
-
Determine athletes’ sweat rates by providing pre and post body weights during practices and competition.
-
Establishing an accurate sweat rate will help determine the fluid needs of individual players during practice and competition to prevent dehydration associated performance deficits.
-
During participation, athletes should aim to minimize fluid losses to keep levels of dehydration <2% of body mass losses. Those with large sweat rates may not be able to replace all fluid losses during participation and in such cases, the remaining fluid deficits must be replaced after practice.
-
Consuming beverages containing carbohydrates and electrolytes (found in sports drinks) increases the ability for the body to retain water and helps the body retain water and helps enhance the ability to stay hydrated.
-
After exercise, athletes should replace all remaining fluid deficits. Also drinking beverages that contain carbohydrates, electrolytes and protein helps retain the water and also provides benefits for muscle recovery after exercise.
-
During intense exercise in the heat, it is imperative that athletes practice appropriate hydration practices to minimize the risk of increased levels of dehydration that can adversely affect performance and increase the risk of heat illness.
SUMMARY
Dehydration of >2% body mass losses can impair performance and have safety implications (i.e., increase the risk of heat illness). In American football, athletes are susceptible to dehydration especially when environmental conditions are extreme. Establishing individualized hydration plans for each athlete and providing proper education on the importance of hydration, both during practice/competition and throughout the day, are important to ensure the athlete’s hydration and resulting safety and performance during football (Table 4).
REFERENCES
Adams, W. M., E.M. Ferraro, R.A. Huggins, and D.J. Casa (2014). Influence of body mass loss on changes in heart rate during exercise in the heat: a systematic review. J. Strength Cond. Res. 28:2380–2389.
Almond, C.D., A.Y. Shin, E.B. Fortescue, R.C. Mannix, D. Wypij, B.A. Binstadt, C.N. Duncan, D.P. Olson, A.E. Salerno, J.W. Newberger, and D.S. Greenes (2005). Hyponatremia among runners in the Boston Marathon. New Eng. J. Med. 352:1550–1556.
Armstrong, L.E., E.C. Johnson, D.J. Casa, M.S. Ganio, B.P. McDermott, L.M. Yamamoto, R.M. Lpez, and H. Emmanuel (2010). The American football uniform: uncompensable heat stress and hyperthermic exhaustion. J. Ath. Train. 45:117–127.
Boden, B.P., I. Breit, J.A. Beachler, A. Williams, and F.O. Mueller (2013). Fatalities in high school and college football players. Am. J. Sports Med. 41:1108–1116.
Buono, M.J., and J.A. Wall (2000). Effect of hypohydration on core temperature during exercise in temperate and hot environments. Eur. J. Physiol. 440:476–480.
Carter, R. (2008). Exertional heat illness and hyponatremia: An epidemiological prospective. Cur. Sports Med. Rep. 7:S20–S27.
Casa, D.J., L.E. Armstrong, S.K. Hillman, S.J. Montain, R.V. Reiff, B.S. Rich, W.O. Roberts, and J.A. Stone (2000). National athletic trainers’ association position statement: fluid replacement for athletes. J. Ath. Train. 35:212–224.
Casa, D.J., R.L. Stearns, R.M. Lopez, M.S. Ganio, B.P. McDermott, S. Yeargin, L.M. Yamamoto, S.M. Mazerole, M.W. Roti, L.E. Armstrong, and C.M. Maresh (2010). Influence of hydration on physiological function and performance during trail running in the heat. J. Athl. Train. 45:147-156.
Casa, D.J., L.E. Armstrong, G.P. Kenny, F.G. O’Connor, and R.A. Huggins (2012). Exertional heat stroke: new concepts regarding cause and care. Cur. Sports Med. Rep. 11:115–123.
Cheuvront, S.N. and R.W. Kenefick (2014). Dehydration: physiology, assessment, and performance effects. Comp. Physiol. 4:257–285.
Cheuvront, S.N., R.W. Kenefick, S.J. Montain, and M.N. Sawka (2010). Mechanisms of aerobic performance impairment with heat stress and dehydration. J. Appl. Physiol. 109:1989–1995.
Craig, A.B. (1968). Exposure time to injury in professional football. Res Quart. 39:789–791.
DeMartini, J.K., J.L. Martschinske, D.J. Casa, R.M. Lopez, M.S. Ganio, S.M. Walz, and E.E. Coris (2011). Physical demands of National Collegiate Athletic Association division I football players during preseason training in the heat. J. Strength Cond. Res. 25:2935–2943.
Deren, T.M., E.E. Coris, D.J. Casa, J.K. DeMartini, A.R. Bain, S.M. Walz, and O. Jay (2014). Maximum heat loss potential is lower in football linemen during an NCAA summer training camp because of lower self-generated air flow. J. Strength Cond. Res. 28:1656–1663.
American football players compared with runners in a hot and humid environment. Br. J. Sports Med. 39:205–211.
Godek, S.F., J.J. Godek, and A.R. Bartolozzi (2005b). Hydration status in college football players during consecutive days of twice-a-day preseason practices. Am. J. Sports Med. 33:843–851.
Godek, S.F., A.R. Bartolozzi, R. Burkholder, E. Sugarman, and C. Peduzzi (2008). Sweat rates and fluid turnover in professional football players: A comparison of National Football League linemen and backs. J. Ath. Train. 43:184–189.
Grandjean, A.C., and N.R. Grandjean (2007). Dehydration and cognitive performance. J. Am. Coll. Nutr. 26:549S–554S.
Greenleaf JE. Problem: thirst, drinking behavior, and involuntary dehydration. Med Sci Sports Exerc. 1992;24(6):645-656.
Grundstein, A.J., C. Ramseyer, F. Zhao, J.L. Pesses, P. Akers, A. Qureshi, L. Becker, J.A. Knox, and M. Petro (2012). A retrospective analysis of American football hyperthermia deaths in the United States. Int. J. Biometeorology 56:11–20.
Huggins, R., J. Martschinske, K. Applegate, L. Armstrong, and D. Casa (2012). Influence of dehydration on internal body temperature changes during exercise in the heat: A meta-analysis. Med. Sci. Sports Exerc. 44:791 (abstract).
Judelson, D.A., C.M. Maresh, J.M. Anderson, L.E. Armstrong, D.J. Casa, W.J. Kraemer, and J.S. Volek (2007a). Hydration and muscular performance: does fluid balance affect strength, power and high-intensity endurance? Sports Med. 37:907–921.
Judelson, D.A., C.M. Maresh, M.J. Farrell, L.M. Yamamoto, L.E. Armstrong, W.J. Kraemer, J.S. Volek, B.A. Spiering, D.J. Casa, and J.M. Anderson (2007b). Effect of hydration state on strength, power, and resistance exercise performance. Med. Sci. Sports Exerc. 39:1817–1824.
Marino, F.E. (2004). Anticipatory regulation and avoidance of catastrophe during exercise-induced hyperthermia. Comp. Biochem. Physiol. Part B, Biochem. Mol. Biol. 139:561–569.
Marino, F.E., D. Kay, and N. Serwach (2004). Exercise time to fatigue and the critical limiting temperature: effect of hydration. J. Therm Biol. 29:21–29.
McCullough, E.A., and W.L. Kenney (2003). Thermal insulation and evaporative resistance of football uniforms. Med. Sci. Sports Exerc. 35:832–837.
Montain, S.J., and E.F. Coyle (1992). Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J. Appl. Physiol. 73:1340–1350.
Montain, S.J., M.N. Sawka, W.A. Latzka, and C.R. Valeri (1998). Thermal and cardiovascular strain from hypohydration: influence of exercise intensity. Int. J. Sports Med. 19:87–91.
Noakes, T.D. (2007). Hydration in the marathon : using thirst to gauge safe fluid replacement. Sports Med. 37:463–466.
Payne, M. (2014, August 13). A high school football player dies after reportedly consuming two gallons each of water and Gatorade. The Washington Post. Retrieved from http://www.washingtonpost.com/blogs/early-lead/wp/2014/08/13/ a-high-school-football-player-dies-after-reportedly-consuming-two-gallons-each-of-water-and-gatorade/
Rosner, M.H. (2009). Exercise-associated hyponatremia. Sem. Nephrol. 29:271–281.
Sawka, M.N., A.J. Young, R.P. Francesconi, S.R. Muza, and K.B. Pandolf (1985). Thermoregulatory and blood responses during exercise at graded hypohydration levels. J. Appl. Physiol. 59:1394–1401.
Sawka, M.N., L.M. Burke, E.R. Eichner, R.J. Maughan, S.J. Montain, and N.S. Stachenfeld (2007). American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 39:377–390.
Shirreffs, S.M. (2005). The importance of good hydration for work and exercise performance. Nutr. Rev. 63:S14–S21.
Stover, E.A., J. Zachwieja, J. Stofan, R. Murray, and C.A. Horswill (2006). Consistently high urine specific gravity in adolescent American football players and the impact of an acute drinking strategy. Int. J. Sports Med. 27:330–335.
Yeargin, S.W., D.J. Casa, D.A. Judelson, B.P. McDermott, M.S. Ganio, E.C. Lee, R.M. Lopez, R.L. Stearns, J.M. Anderson, L.E. Armstrong, W.J. Kraemer, and C.M. Maresh (2010). Thermoregulatory responses and hydration practices in heat-acclimatized adolescents during preseason high school football. J. Ath. Train. 45:136–146.